Infective endocarditis (IE) describes the infection of the inner-most layer of the heart, the endocardium.
Pathophysiology
There are two main components to developing IE. Firstly, an abnormal, damaged endocardium is thought to be the first step in the pathophysiology of IE as damage to the endothelium results in clot formation, which serves as a nidus for bacterial colonisation.
Secondly, bacteria need to be present in the blood (bacteraemia), and these bacteria have to be capable of adhering and colonising the endocardium. This can occur through intravenous drug use, poor dental hygiene, cardiac surgery or an open wound. Bacteria can adhere to the aforementioned clot and form a vegetation.
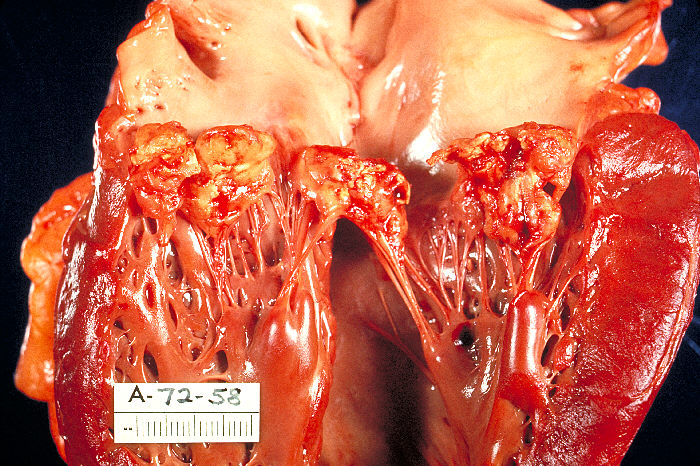
IE vegetations are problematic as they disrupt the normal mechanism of valves, thus resulting in valvular regurgitation. They can also cause other problems including periaortic abscesses and congestive heart failure due to valvular dysfunction. Alternatively, if the vegetations embolise they can cause ischaemic strokes, pulmonary emboli, splenic emboli which result in splenic abscesses, renal emboli which can result in haematuria and more.
See page for author, Public domain, via Wikimedia Commons
Infective Endocarditis Vegetations on the Mitral Valve
Common pathogens which can cause IE include:
- Staphylococcus aureus
- Streptococcus viridans: Associated with dental extractions
- Staphylococcus epidermidis
- Enterococci
- Streptococcus bovis
- Candida species
Risk Factors
- Artificial heart valve
- IV drug use
- Rheumatic heart disease
- Congenital heart disease
- Valve disease e.g. mitral valve prolapse or bicuspid aortic valve
Clinical Features
A new heart murmur on auscultation with fever should raise clinical suspicion for IE. Symptoms may also include malaise, arthralgia, headaches, rigors and night sweats. Signs include:
- Janeway lesions: Non-tender lesions on palms or soles
- Osler’s nodes: Painful lesions on the hands and feet
- Roth spots: Type of retinal haemorrhages
- Splinter haemorrhages: Subungual brown/red lesions
Modified Duke’s Criteria
The modified Duke’s criteria can be used to diagnose IE. It consists of major and minor criteria, and the major criteria can be thought of as bacteraemia related and endocardium related. 2 major criteria, 1 major + 3 minor OR 5 minor criteria confirm the diagnosis. The following is a summary of the Modified Duke’s Criteria:
Major Criteria – Blood Cultures
- Positive for typical organisms in 2 separate cultures OR
- Persistently positive blood cultures
- Single positive culture for Coxiella burnetii
Major Criteria – Endocardium
- Positive echocardiogram for signs of IE e.g. vegetations
- New valvular regurgitation
Minor Criteria:
- Predisposing factor e.g. IV drug use or heart condition
- Positive blood culture that does not meet the major criteria
- Immunological phenomena: Osler’s nodes, Roth spots, glomerulonephritis
- Fever greater than or equal to 38.0C
- Vascular phenomena: Janeway lesions, emboli
Investigations
Bedside
- Urinalysis: Checking for haematuria
- ECG: Check for heart block which can occur with aortic root abscess
Bloods
- Full blood count: May show normocytic anaemia and neutrophilia
- ESR and CRP: Raised
- Urea and electrolytes and liver function test useful for baseline
- Blood cultures: 3 separate sets of cultures, each from different sites need to be taken. Some patients can, however, be culture negative. Organisms such as Coxielle burnetti, Chalmydia and Legionella are some species which can cause a negative culture.
Imaging
- Transthoracic echocardiogram: Useful for visualising vegetations and abnormal valvular function. However, it is less sensitive than transoesophageal echo.
- Transoesophageal echocardiogram: More sensitive but also more invasive. Useful if there is suspicion of an aortic root abscess.
Management
Treatment of IE is mainly with IV antibiotics – the precise management plan varies so consult local guidelines, microbiologist and cardiologist based on cultures. Examples of blind therapy i.e. prior to confirmed culture includes:
- Native valve or a prosthetic valve which was implanted at least a year ago:
- Not penicillin allergic: Ampicillin + Flucloxacillin + Gentamicin
- Penicillin allergic: Vancomycin + Gentamicin
- Prosthetic valves: Vancomycin + Gentamicin + Rifampicin
Patients with heart failure due to severe valvular regurgitation or uncontrolled infection may require cardiac surgery.
Complications
- Ischaemic stroke
- Congestive heart failure
- Valvular insufficiency
- Pericarditis
- Aortic root abscess
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5240923/
https://www.utmb.edu/pedi_ed/CoreV2/Cardiology/cardiologyV2/cardiologyV219.html
https://www.sciencedirect.com/science/article/pii/S0146280605001854?via%3Dihub
https://www.mayoclinic.org/diseases-conditions/endocarditis/symptoms-causes/syc-20352576
http://www.nnuh.nhs.uk/publication/treatment-of-endocarditis-jcg0006-v2-1/
https://emedicine.medscape.com/article/216650-overview#a3
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4632890/