Thyrotoxicosis is the condition where there are excessive levels of circulating thyroid hormone. When these high levels of hormone originate from excess production by the thyroid gland, it is known as hyperthyroidism.
Thyroid Gland Structure and Function
The thyroid gland is a butterfly shaped gland found anterior to the trachea in the neck. It produces thyroid hormone which has a widespread role in the body affecting multiple bodily functions including metabolism and growth.
Three main hormones are produced by the thyroid:
- Triiodothyronine (T3) – this is the active form of the hormone.
- Tetraiodothyronine (T4) - T4 is converted in the peripheries in certain tissues including kidney, liver and muscle tissues.
- Calcitonin
The vast majority of T3 and T4 hormone is bound to transport proteins in the serum, including thyroxine-binding globulin (TBG) and albumin. It is the amount of free (unbound) T3 hormone which is truly active.
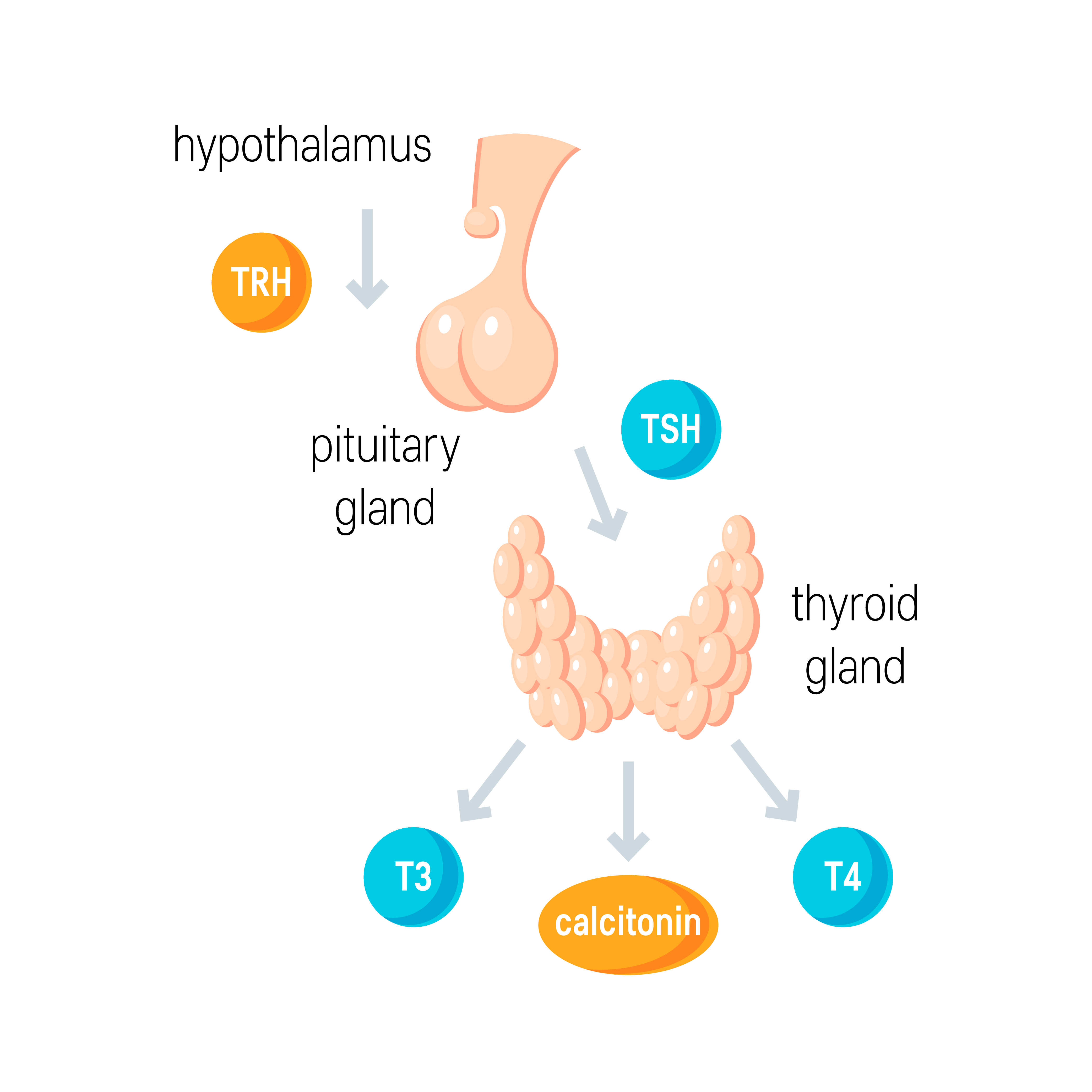
Thyroid Hormonal Axis
Thyroid hormone homeostasis begins at the hypothalamus. The axis works in the following way:
- The periventricular nucleus (PVN) of the hypothalamus releases thyroid releasing hormone (TRH) into the hypothalamo-hypophyseal portal system to get to the anterior pituitary gland.
- TRH stimulates release of thyroid stimulating hormone (TSH) from the anterior pituitary gland.
- TSH binds to receptors on follicular cells of the thyroid gland, resulting in increased levels of serum T3 and T4.
- T3 and T4 work to increase metabolic and cellular activity. Some actions of their actions include:
- Increasing heart rate
- Increasing gut motility
- Increasing lipolysis
- Increasing metabolism of carbohydrates i.e., upregulation of glycogenolysis (breaking down of glycogen) and gluconeogenesis (synthesis of glucose)
- TRH also stimulates prolactin production from the anterior pituitary which can cause lactation and growth of breast tissues.
Copyright Medic in a Minute 2021
Thyroid Hormonal Axis
Causes
The most common cause of hyperthyroidism is Grave’s disease, an autoimmune condition whereby serum IgG antibodies known as thyroid stimulating hormone receptor antibodies bind to TSH receptors on the thyroid gland which subsequently stimulates thyroid hormone production. Grave’s disease is associated with other autoimmune conditions including type 1 diabetes mellitus and Addison’s disease.
Other causes include:
- Solitary toxic adenoma/nodule: A single adenoma or nodule on the gland is producing excessive quantities of thyroid hormone.
- Multinodular goitre
- Thyroiditis: Inflammation of the thyroid gland. There are two main types:
- Subacute (De Quervain’s) thyroiditis: Inflammation of the thyroid gland typically following a viral infection. The thyroid is usually tender to touch, and patients may complain of pain in the neck.
- Post-partum thyroiditis: Inflammation of the thyroid gland following childbirth. This tends to be painless with milder symptoms.
- Excess iodine: This can be iatrogenic e.g., from a contrast medium, over-treatment of hypothyroidism, or perhaps due to drugs such as amiodarone.
Clinical Features
Thyroid hormone is involved in metabolism and therefore, increased quantities of the hormone can lead to general ‘speeding up’ of multiple bodily functions.
- Weight loss
- Heat intolerance and sweating: May dress inappropriately for the time of year e.g. wearing thin clothes in winter
- Increased appetite
- Diarrhoea
- Irritability
- Anxiety
- Fine tremor
- Palpitations
- Alopecia
- Oligomenorrhoea or Amenorrhoea
Examination features include:
- Palmar erythema
- Proximal muscle weakness (ask patients to stand up whilst crossing their arms on their chest. Patients with significant proximal myopathy will struggle to stand up)
- Tachycardia
- Atrial fibrillation
- Goitre (a visible swelling of the neck due to an enlarged thyroid gland) may be found and a bruit may also be auscultated over the thyroid gland.
- Lid lag: Normally, when you look up at the ceiling and then move your eyes to look at your feet, your eyeball and upper eyelid will both move downwards at the same time. In thyrotoxicosis however, a change occurs whereby the upper eyelid is higher than it should be when the eyeball is looking downwards. This looks like a 'lag' of the eyelid, when asking the patient to look down.
- Lid retraction: Normally, the upper eyelid conceals the sclera between the superior limbus and upper lid, covering part of the iris. In lid retraction, this sclera is visible leading to a staring appearance of the eyes.
- Pretibial myxoedema: TSH receptor antibodies are capable of activating T cells which subsequently release inflammatory cytokines that cause activation of dermal fibroblasts leading to excess GAG deposition in the skin. This leads to swelling and thus the classic waxy and lumpy appearance of pretibial myxoedema which is most commonly seen on the pretibial regions.
- Thyroid acropachy: Swelling of distal digits which can look similar to clubbing
Herbert L. Fred, MD and Hendrik A. van Dijk, CC BY 2.0 , via Wikimedia Commons
Pre-Tibial Myxoedema and Thyroid Acropachy
Grave’s Disease Features
In Grave’s, the TSH receptor antibodies as well as other inflammatory cytokines cause retro-orbital activation of fibroblasts and precursor adipocytes. The former leads to the production of excess glycosaminoglycans (GAGs) which trap water and lead to excessive swelling of the extra-ocular muscles – this swelling, over long periods of time, can lead to fibrosis of the extra-ocular muscles. Excessive fat is also deposited retro-orbitally. This process leads to the following signs:
- Peri-orbital oedema
- Exophthalmos/Proptosis: This is the bulging of the eyes (due to the retro-orbital excess fat growth which pushes the eye forward)
- Ophthalmoplegia and Diplopia: There is restricted movement of the eye due to the swollen extra-orbital muscles and thus patients may complain of double vision
- Eye irritation
- Photophobia
Jonathan Trobe, M.D. - University of Michigan Kellogg Eye Center, CC BY 3.0 , via Wikimedia Commons
Proptosis and Lid Retraction - Graves Eye Disease
Investigations
Bedside
- Observations
- ECG: Atrial fibrillation and tachycardia
Bloods
- Thyroid function test
- Serum TSH receptor antibodies: 98% sensitive and 99% specific for Grave’s disease
- Thyroid peroxidase antibodies: These are present in approximately 75% of patients with Grave’s disease (they can also be present in Hashimoto’s thyroiditis)
- CRP/ESR for thyroiditis
- FBC, U&E and LFTs: Baseline, particularly if wanting to start anti-thyroid therapies
Imaging
- Radioisotope scan: Observing uptake of technetium pertechnetate (Tc-99m a substance which closely mimics radioactive iodine) by the thyroid gland which can help to determine a diagnosis when Grave’s is unlikely.
- In Grave’s disease, the uptake is diffuse throughout the gland.
- If there is a single toxic nodule or adenoma, it will be seen as a ‘hot’ nodule on the scan i.e. the uptake of Tc-99m is higher by that region compared to the rest of the thyroid gland.
- Under NICE guidelines, radioisotope scans are usually considered if TSH receptor antibodies are negative.
- CT or MRI scan of the orbits: May show enlarged extra-ocular muscles in Grave’s disease
- Ultrasound of Thyroid Gland: As per NICE guidance, this is only considered if there is a palpable nodule on the thyroid gland.
Management
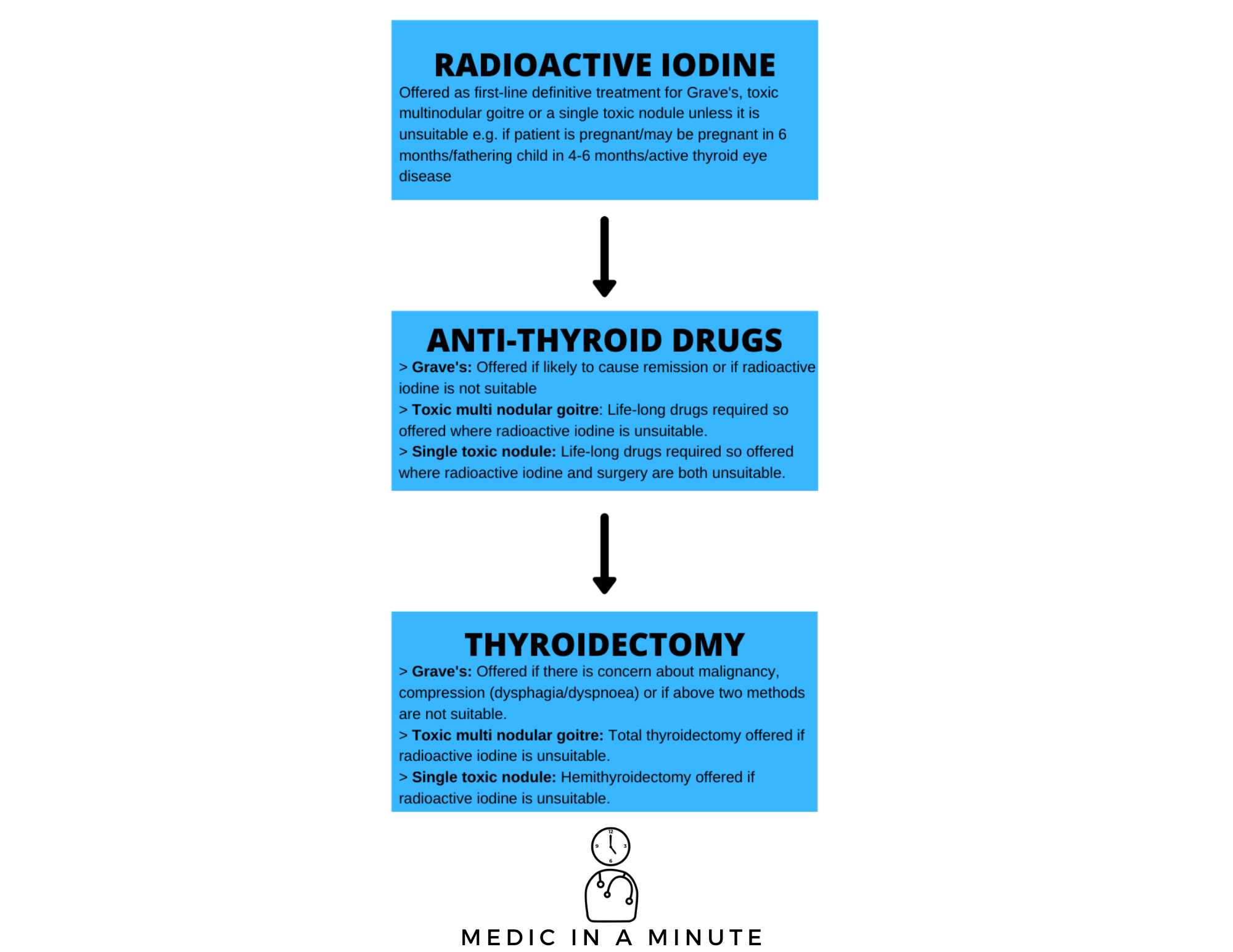
NICE Guidelines recommend either radioactive iodine or an antithyroid drug as first line definitive treatment. If either of these are not suitable or if there is suspicion of thyroid cancer, a total thyroidectomy can be offered.
Should the thyroid gland become significantly large, it can cause compression of nearby structures which could cause dysphagia and dyspnoea – in these cases, a total thyroidectomy is usually performed. The salient points from the NICE guidelines on managing hyperthyroidism have been summarised in the below graphic.
Copyright Medic in a Minute
Hyperthyroidism/Thyrotoxicosis Management
Radioactive Iodine
Radioactive iodine is taken up by the thyroid gland and causing subsequent destruction of the tissue, thus treating the condition. Patients may well develop hypothyroidism following treatment and require levothyroxine.
It cannot be used in certain circumstances e.g. if the patient is pregnant/trying to become pregnant within the next 6 months, or if the patient is planning on fathering a child in the next 4-6 months, or in instances of active Graves' thyroid eye disease, as it can worsen symptoms.
Antithyroid Drugs
Patients should have a full blood count and liver function test before antithyroid drugs are started.
There are two main drugs which are recommended by NICE – carbimazole and propylthiouracil.
Carbimazole
Carbimazole is used for 12-18 months in one of the following methods:
- Block and Replace: Carbimazole and levothyroxine are offered together in order to avoid iatrogenic hypothyroidism
- Titration: Carbimazole is given at a specific dose for 4 weeks, and then thyroid function is reviewed, and the dose is adjusted accordingly. This is usually considered when patients are being offered life-long therapy.
A major side effect of carbimazole is agranulocytosis and liver dysfunction. Although full blood counts and liver function tests are not routinely monitored, if patients do develop infection or have symptoms of an infection such as a sore throat, they should immediately stop the drug, report the symptom and get an urgent full blood count. Carbimazole also carries a risk of acute pancreatitis
Carbimazole is largely contraindicated in the first trimester pregnancy due to the risk of congenital malformations, and it is advised that effective contraception be used whilst women of childbearing potential are on the treatment. It is, however, used for the remainder of pregnancy.
Propylthiouracil
Propylthiouracil can be used as an alternative to carbimazole in the following circumstances:
- History of adverse reaction to carbimazole
- If a patient has a medical history of pancreatitis
- Pregnant or intend to become pregnant in the next 6 months as its safer than carbimazole in the first trimester
Monitoring
Patients should have their thyroid function tests monitored every 6 weeks for the first 6 months following radioactive iodine treatment until TSH normalises. Patients who undergo a total thyroidectomy will require thyroid hormone replacements in the form of levothyroxine.
References
https://www.ncbi.nlm.nih.gov/books/NBK557646/
https://www.ncbi.nlm.nih.gov/books/NBK500006/
https://www.statpearls.com/sp/pa/30167/
https://www.sciencedirect.com/topics/medicine-and-dentistry/von-graefes-sign
https://www.dermnetnz.org/topics/pretibial-myxoedema/
https://www.ncbi.nlm.nih.gov/books/NBK448195/
https://www.racgp.org.au/afp/2012/august/thyroid-scans/
https://www.gov.uk/drug-safety-update/carbimazole-increased-risk-of-congenital-malformations-strengthened-advice-on-contraception
https://www.nice.org.uk/guidance/ng145/chapter/Recommendations#investigating-suspected-thyroid-dysfunction-or-thyroid-enlargement
https://www.gov.uk/drug-safety-update/carbimazole-risk-of-acute-pancreatitis
Oxford Handbood of Clinical Medicine 10th Edition
https://www.btf-thyroid.org/thyroid-in-pregnancy-faqs