Acute rheumatic fever is a condition triggered by a bacterial infection with group A streptococcus bacteria.
Pathophysiology
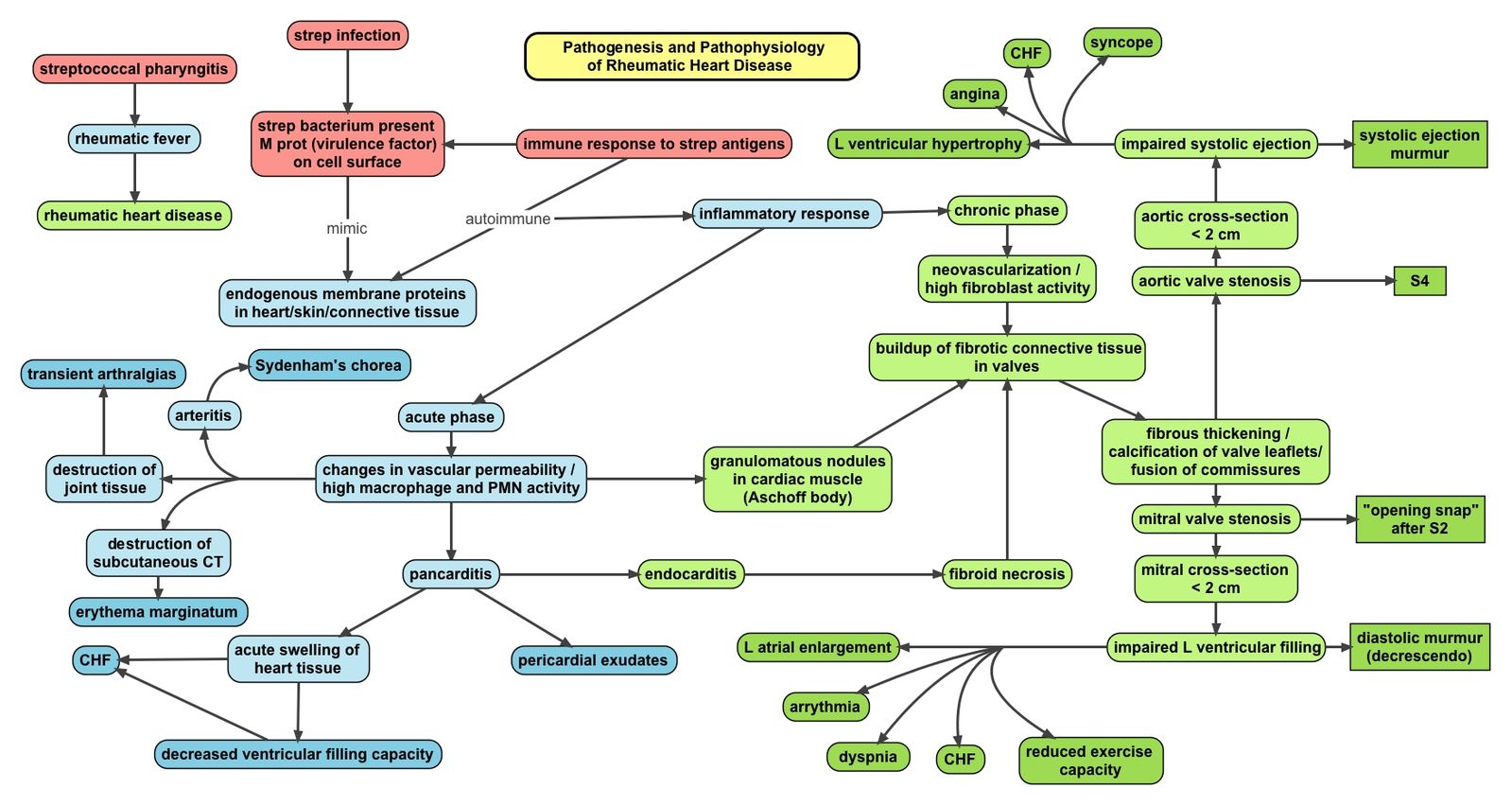
Patients will have had an infection with group A streptococcus bacteria e.g. streptococcus pyogenes, prior to developing rheumatic fever. The body produces antibodies against the antigens on the bacteria – however, these antibodies cross-react with self-tissues including the endocardium, myocardium, pericardium, joints and skin resulting in inflammation and symptoms.
Oxynthes, Public domain, via Wikimedia Commons
Pathophysiology of Rheumatic Heart Disease
Clinical Features
- Fever
- Arthritis and arthralgia: One of the most major presenting features of the condition. Typically affects the large joints.
- Fatigue
- Carditis: Can manifest in various ways. Patients can develop heart failure if there is profound valvular regurgitation or in case of dysfunctional myocardium.
- Although all the layers of the heart can be affected, the endocarditis is often the main clinical manifestation. Patients can present with mitral or aortic regurgitation.
- Pericardial rub in case of pericarditis
- Dyspnoea: Because of heart failure or pericardial effusions
- Chest pain
- Peripheral oedema: Due to heart failure
- Chorea: This is known as Sydenham’s chorea or St Vitus’s dance in the context of rheumatic fever, characterised by purposeless involuntary movements which usually affect one side of the body more than the other. It is a later manifestation and appears months after the acute episode.
- Cutaneous:
- Subcutaneous nodules occurring over joints and the back of the scalp.
- Erythema marginatum: An annular rash which is usually found on the upper arms, legs and trunk.
Modified Jones Criteria
The revised Jones criteria are used for diagnosing rheumatic fever. There are two versions of the criteria – either for low-risk populations (USA, Europe, high-income countries) or high-risk populations (Oceania, Africa, low-income countries). 2 major criteria OR 1 major + 1 minor, alongside evidence of a recent streptococcal infection (e.g. a positive throat culture/elevated or rising strep antibody titre) confirm the diagnosis.
| Low-Risk | High-Risk |
| Major Criteria | - Carditis
- Polyarthritis
- Chorea
- Erythema marginatum
- Subcutaneous nodules
| - Carditis
- Polyarthritis or monoarthritis
- Chorea
- Erythema marginatum
- Subcutaneous nodules
|
| Minor Criteria | - Polyarthralgia
- Fever >38.5 C
- Raised ESR (>60mm/hr) and CRP (>3mg/L)
- Prolonged PR interval
| - Polyarthralgia
- Fever >38 C
- Elevated ESR (>30mm/hr) and CRP (>3mg/L)
- Prolonged PR interval
|
Note – you cannot count both arthritis as a major criterion and arthralgia as a minor criterion.
Investigations
Bedside
Bloods
- ESR and CRP
- Antistreptolysin O antibody titre: Typically raised following a streptococcal infection
Imaging
- Echocardiography: Looking for valvular regurgitation
- Chest X-ray: May see cardiomegaly or signs of congestive cardiac failure
Management
- Bed rest can help with the arthritis and reduces strain on the heart
- If heart failure develops, it should be treated. More severe valvular dysfunction may necessitate valve replacement.
- Antibiotics can be prescribed to eradicate any residual infection.
- Analgesia to help relieve arthritis and carditis pain – aspirin is usually used for this, but NSAIDs can be used instead in case of contraindications.
Complications
Patients can develop chronic rheumatic heart disease which results in permanent damage to the heart valves as a result of inflammation. This most commonly affects the mitral valve (50-60%), followed by the aortic valve. Patients can develop regurgitation or stenosis of the valve, although stenosis typically occurs years following the initial acute episode. Patients may require valve repair or valve replacement.
References
https://www.ncbi.nlm.nih.gov/books/NBK425394/
https://www.ncbi.nlm.nih.gov/books/NBK538286/
https://dermnetnz.org/topics/rheumatic-fever/
https://www.medscape.com/answers/236582-31419/what-are-the-jones-criteria-for-diagnosis-of-acute-rheumatic-fever-arf
https://www.ncbi.nlm.nih.gov/books/NBK425394/
https://patient.info/doctor/rheumatic-fever-pro