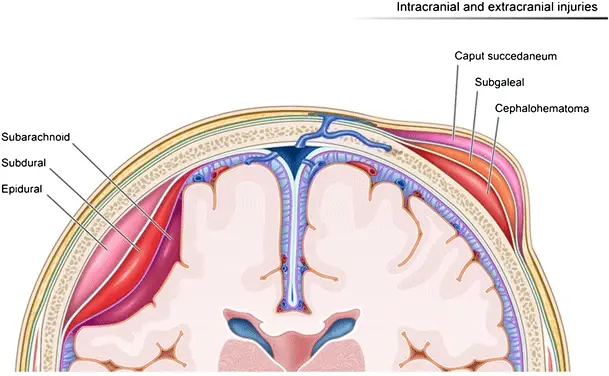
A subarachnoid haemorrhage (SAH) is when there is bleeding into the subarachnoid space – this is the spider-web like space between the arachnoid mater and pia mater.
Causes and Risk Factors
- Trauma
- Ruptured Berry Aneurysm: The most common cause in atraumatic SAHs. These are are dilations in the walls of the vessels of the brain. These tend to occur at junctions of the circle of Willis. The larger an aneurysm, the greater risk of it rupturing.
- Arteriovenous malformations: These usually occur when an abnormal connection (fistula) forms between an arterial vessel and a venous vessel. Blood from the higher pressured arterial system ends up flowing through veins which are not designed to handle such high pressures, leading to an abnormality of the vessels. If they haemorrhage, they can lead to a subarachnoid haemorrhage.
- Polycystic kidney disease: Increases risk of forming berry aneurysms
Nadezdha D. Kiriyak, CC BY 4.0 , via Wikimedia Commons
Meningeal Layers
Clinical Features
- Thunderclap headache:
- Sudden onset
- Usually occipital
- Extremely excruciating– usually described as the worst headache of a patient’s life.
- Loss of consciousness
- Vomiting
- Seizures
- Meningism: Neck stiffness/rigidity and photophobia
- Drowsiness/Reduced GCS
Investigations
Bedside
- Neuro-observations
- ECG: Can show various changes such as T wave inversion or ST-segment changes
Bloods
- FBC, U&E, Bone Profile: Baseline
- Clotting studies: Abnormal coagulation may require correction
- Group and save: Pre-operative
Imaging
- CT Head: Haemorrhaging will be visible in the sulci of the brain, particularly the Sylvian fissure. Alternatively, it may be apparent around the area of the circle of Willis.
- CT Angiogram: Sensitive for assessing ruptured aneurysms
- Magnetic resonance angiogram: If CTA doesn’t show an aneurysm but there is high suspicion of one
Special Tests
- Lumbar Puncture: If the CT is negative but there is high clinical suspicion of a subarachnoid haemorrhage, a lumbar puncture can be done.
- Since the bleeding is in the subarachnoid space which is where the CSF is, a LP should show blood.
- If done 12 or more hours after the onset of the headache, a positive sample will be xanthochromic i.e. it will have a yellow colour due to the breakdown of red blood cells into bilirubin.
William Laborde, MD, Brandon Mong, MD, and Joel Mosley, MD, CC BY 4.0 , via Wikimedia Commons
Xanthochromia Sample
Management
Medical
- Airway management: Airway adjuncts or intubation if the patient is not maintaining their airway
- Nimodipine: Prevents vasospasm that would otherwise result in ischaemia
- Blood Pressure Control: Blood pressure needs to be controlled to prevent worsening of bleeding e.g. with IV bolus/infusion of labetalol. However, this must be carefully balanced to ensure adequate MAP is maintained to prevent cerebral ischaemia.
- IVF: To ensure adequate cerebral perfusion
Surgical
- Endovascular coiling: Endovascular coiling involves placing platinum coils into the aneurysm to promote thrombosis and thus seal off blood flow to the aneurysm.
- Clipping: Involves placing metal clips at the neck of the aneurysm to seal off blood flow to the aneurysm.
Complications
- Rebleeding: SAH with an underlying aneurysm have a risk of rebleeding following surgery.
- Vasospasm: Spasm of vessels resulting in ischaemia to the brain.
- Acute hydrocephalus
- Hyponatraemia
References
https://emedicine.medscape.com/article/1164341-treatment#d11
Oxford Handbook of Clinical Medicine