An aortic dissection occurs when there is a tear in the wall of the aorta, resulting in pain and various other symptoms.
Risk Factors
- Hypertension
- Atherosclerosis
- Marfan’s syndrome
- Pregnancy
- Trauma
- Iatrogenic e.g. from cardiac catherization/aortic valve replacement/mitral valve replacement/percutaneous insertion of a stent
- Things which cause a sudden increase in blood pressure e.g. cocaine use, ecstasy
- Bicuspid aortic valve
Pathophysiology
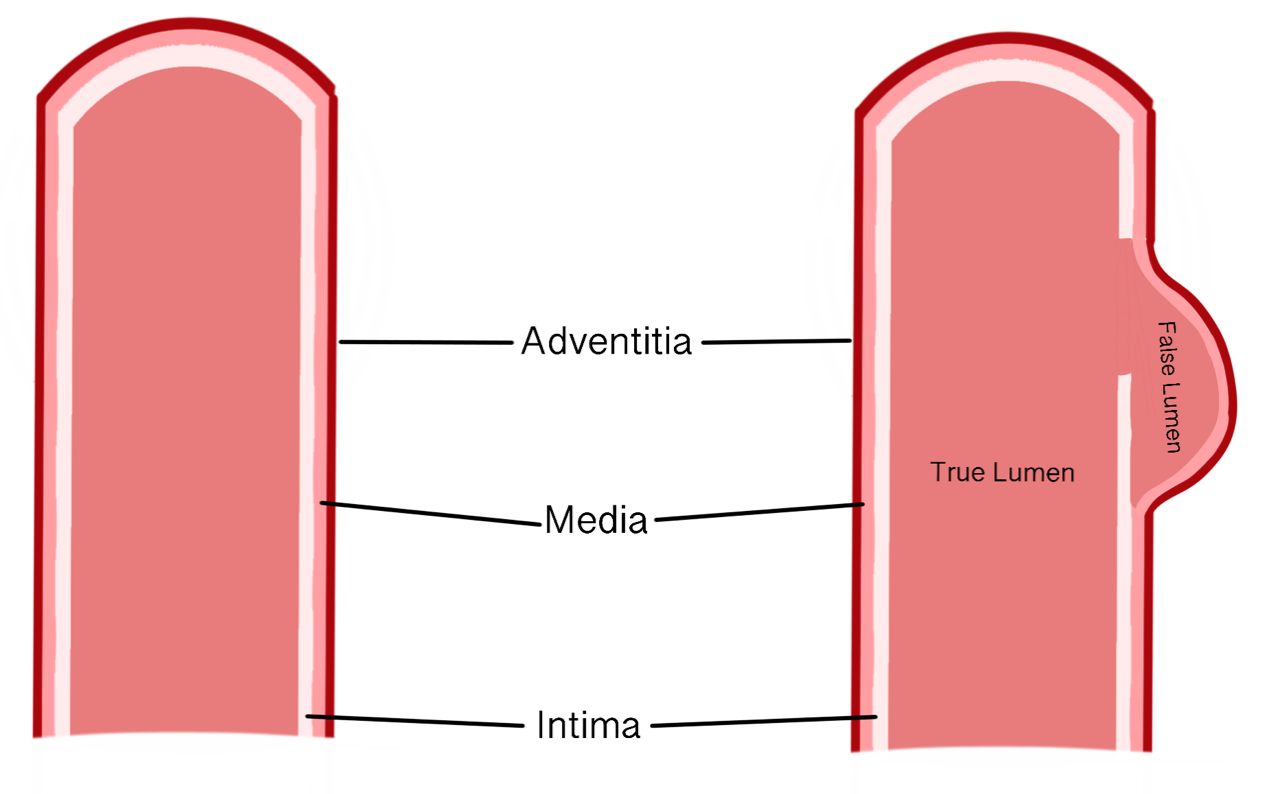
The wall of the aorta has three layers (outer to inner): adventitia, media and intima. A dissection occurs when there is a tear in the intima i.e. in the innermost layer, resulting in blood flowing into the space between the intima and the media which creates a false lumen.
Copyright Medic in a Minute 2021
Diagram of Artery on the Left with Dissection on the Right
The false lumen can become so large that it can occlude the flow of blood through the true lumen.
Classification
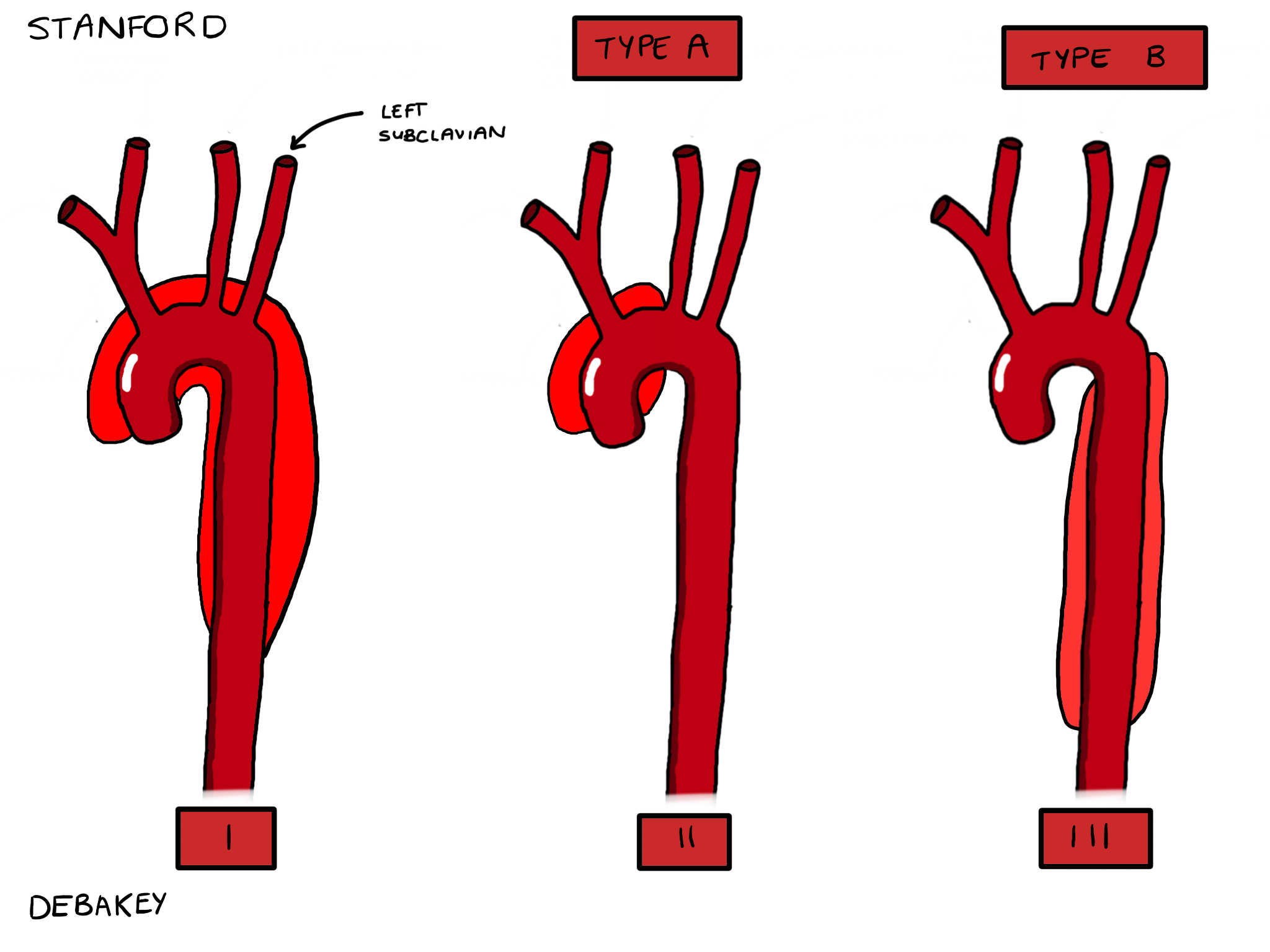
The Stanford and DeBakey classification systems are widely used to classify aortic dissections.
Stanford
- Type A: Dissection which affects the ascending aorta
- Type B: Dissection which affects descending aorta (distal to the origin of the left subclavian artery)
Copyright Medic in a Minute 2021
Stanford and DeBakey Classifications
DeBakey
- Type I: Originates in the ascending aorta and extends to at least the aortic arch but it can extend past the arch as well
- Type II: Originates and only involves the ascending aorta
- Type III: Originates in the descending aorta and extends distally.
- If it remains above the level of the diaphragm, it is a type IIIa
- If it extends below the level of the diaphragm, it is a type IIIb
Clinical Features
- Sudden onset chest pain which can be described as a ‘tearing’ sensation
- Back pain between the scapulae
- Syncope
- Patients with dissections tend to be hypertensive, unless the dissection has ruptured or there is a cardiac tamponade in which case, they may be hypotensive
- Signs suggesting a cardiac tamponade (remember Beck’s triad):
- Hypotension
- Muffled heart sounds
- Raised jugular venous pressure
- Difference in blood pressure in left and right arm
- Aortic regurgitation murmur i.e. crescendo diastolic murmur
Investigations
Bedside
- ECG: Rules out other causes of chest pain such as a myocardial infarction
- Observations
Bloods
- FBC, U&E, LFT, Clotting: Baseline
- G&S and XM
Imaging
- Chest x-ray: Distorted aortic knuckle, widened mediastinum, haemothorax
- CT or MR angiogram chest, abdomen and pelvis: Identification of the intimal flap and fluid (blood) in the pericardium
- Echocardiogram: May show aortic regurgitation, dilated aortic root or a free intimal flap within the lumen of the aorta. A transoesophageal echo is more sensitive than a transthoracic echo, but the latter may be more accessible particularly at the bedside of an acutely unwell patient.
Management
Supportive Management
General supportive management i.e. analgesics for pain, fluid resuscitation, oxygenation, IV access and blood pressure support are important. Patients with dissection may be managed through permissive hypotension i.e. ensuring the systolic blood pressure remains between 100-120mmHg in order to prevent further progression of the dissection with high blood pressures. The heart rate is also controlled, ideally between 60-80 beats/minute. This is usually done through beta-blockers, or non-dihydropyridine calcium channel blockers if beta-blockers are contraindicated.
Definitive Treatment
Definitive treatment depends on the Stanford classification of the dissection. Type A dissections require urgent cardiothoracic surgery to replace the ascending aorta with a prosthetic graft.
Patients with a Type B dissection can be managed medically if there is no threat to end-organs such as the kidneys with blood pressure and heart rate control through beta-blockers/non di-hydropyridine calcium-channel blockers. Complicated dissections e.g. where there is tissue ischaemia may require surgery which is usually done through endovascular stent placement.
Complications
It is possible for the dissection to rupture completely, resulting in bleeding into bodily cavities. Bleeding into the pericardial sac can result in haemopericardium, cardiac tamponade and subsequent death. Bleeding into the thorax can result in a haemothorax.
It is also possible to develop ischaemia to the organs e.g. brain resulting in stroke, or limbs.
References
https://www.rcemlearning.co.uk/reference/aortic-dissection/#1568112704060-230d2cb2-b919
https://www.ncbi.nlm.nih.gov/books/NBK441963/
https://www.medscape.com/answers/756835-163960/what-is-the-stanford-classification-of-acute-aortic-dissection-aad
https://www.bmj.com/content/344/bmj.d8290