A stroke describes a condition where there is a sudden disruption to blood supply to the brain, resulting in tissue death and a subsequent neurological deficit.
Cerebrovascular Accident
You might hear strokes being referred to as cerebrovascular accidents (CVAs). There are two main types:
- Ischaemic: A lack of blood supply results in death of brain tissue (known as infarction). These account for the vast majority of strokes, and this is what we’re focusing on in this set of notes.
- Haemorrhagic: Bleeding results in death of brain tissue.
Blood Supply
Understanding the vascular supply of the brain is helpful in order to identify where the ischaemia is. There are three main points to understand here –
1) The Circle of Willis
2) Vascular Territories
3) Anterior vs Posterior Circulation
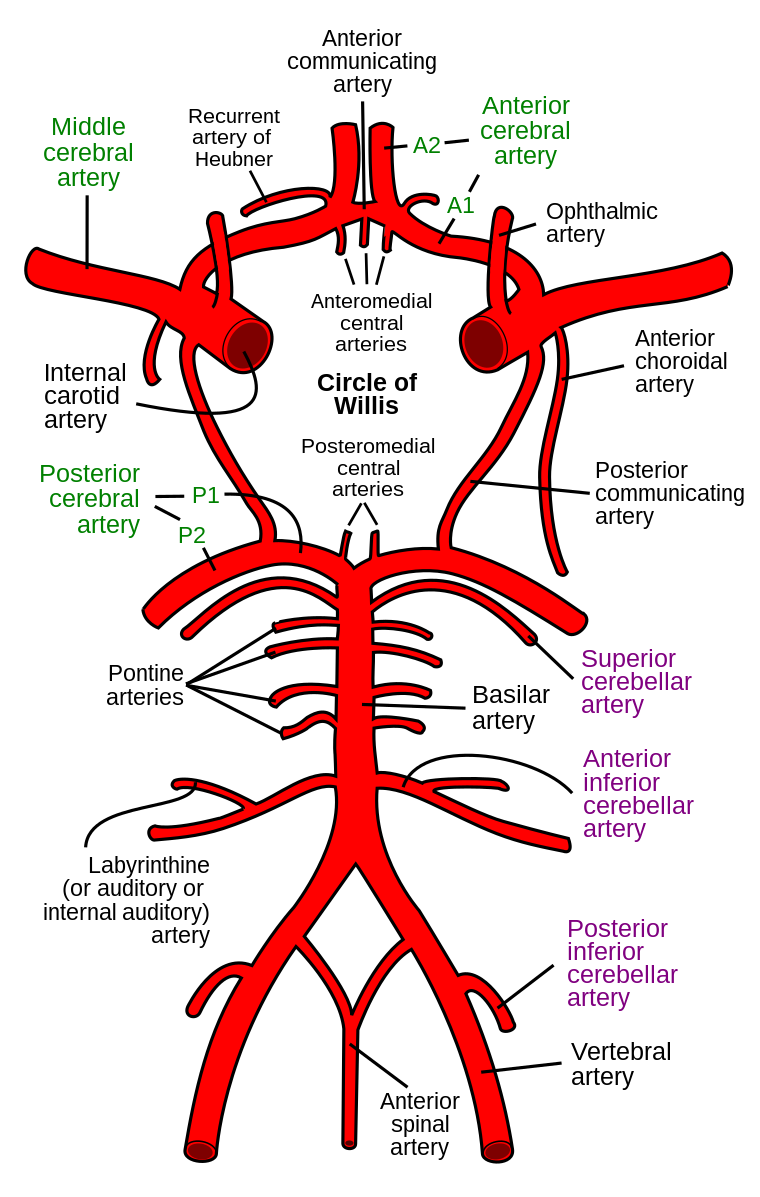
The Circle of Willis
Two pairs of major arteries, the vertebral arteries and internal carotid arteries, anastamose in the cranium to form the Circle of Willis, which branches off to supply the majority of the brain.
Rhcastilhos, Public domain, via Wikimedia Commons
Circle of Willis
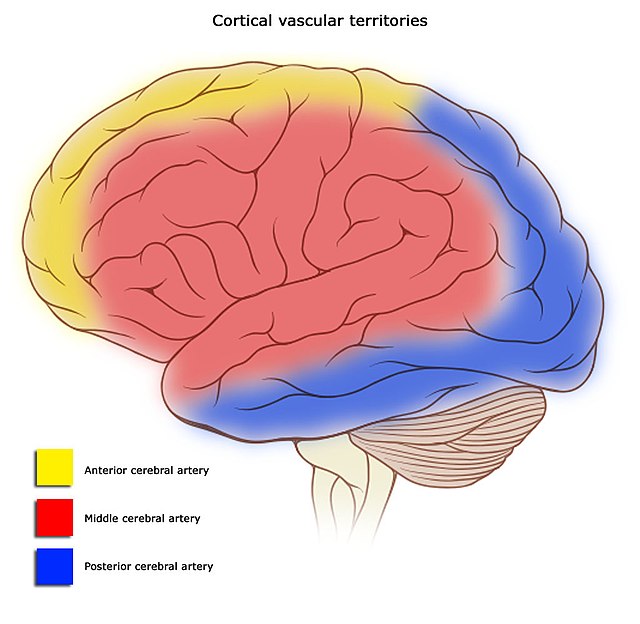
Vascular Territories
There are major blood vessels formed by the Circle of Willis which are important to know about in the context of ischaemic stroke, as these vessels supply the majority of the brain. These are the anterior, middle and posterior cerebral arteries.
Each of these vessels have vascular territories i.e. parts of the brain that they’re known to supply. These vascular territories are helpful because they a) help you understand why you get certain symptoms based on what part of the brain is affected and b) have different appearances radiologically.
The diagram below shows the vascular territories of the respective arteries. For example, when you get a middle cerebral artery ischaemic stroke, you will radiologically see the vascular territory of the middle cerebral artery affected.
derivative work: Frank Gaillard (talk)Brain_stem_normal_human.svg: Patrick J. Lynch, medical illustrator, CC BY-SA 3.0 , via Wikimedia Commons
Cerebral Vascular Territories
Anterior and Posterior Circulations
The brain can be split majorly into the anterior and posterior circulation, which the Circle of Willis connects up together.
- Anterior Circulation: Formed by the anterior and middle cerebral arteries and supplies the anterior part of the brain
- Posterior Circulation: Posterior cerebral, basilar and vertebral arteries and supplies the posterior part of the brain
Pathophysiology
- Just like every other organ, your brain requires blood flow to function normally. Reduced blood flow (ischaemia), will start to cause cell dysfunction.
- In the context of an ischaemic stroke, certain parts of the areas of the brain are described as the ischaemic core regions – these parts are already infarcted, or are going to infarct, when the patient is assessed.
- The penumbra surrounds the ischaemic core, and it is the region of tissue which can potentially be salvaged if blood flow is quickly restored.
- The whole principle of ischaemic stroke management is to get rid of the cause of ischaemia, with the hopes of salvaging this penumbral tissue.
- Ischaemia causes problems in a lot of different ways. We won’t go through everything here, but it’s nice to understand the basic principles so you understand what’s happening when you see a patient in front of you.
- Cytotoxic Oedema: Na-K channels (3 sodium ions out of the cell, 2 potassium ions into the cell) will stop functioning in ischaemic conditions due to a lack of glucose, resulting in higher levels of intracellular sodium, which draws water into the cell resulting in cytotoxic oedema. This oedema puts pressure on surrounding tissues and vessels, resulting in damage to the blood-brain barrier which further contributes to inflammation secondary to infiltration of immune cells and cytokines.
- Vasogenic Oedema: Due to the disruption of the blood-brain barrier, blood vessels in the brain essentially get more leaky and start spilling out intravascular components such as proteins into the brain tissue. This disruption to the blood-brain barrier is thought to be one of the mechanisms of haemorrhagic transformation of an ischaemic stroke.
- All this oedema can contribute to increased intracranial pressure which can both reduce blood flow in the brain further, and also potentially result in brain herniation.
- Due to an increase in anaerobic metabolism in a hypoxic environment, there will be reduced ATP production. Cells will struggle to meet their metabolic demands, resulting in cell death.
Transient Ischaemic Attacks
It is important to note that in stroke, clinical features of neurological deficit are present for more than 24 hours. If these features were to resolve in less than 24 hours, the patient is said to have had a transient ischaemic attack (TIA). These are exactly what they say on the tin – transient drops in blood supply which don’t actually result in any tissue death, hence no permanent neurological deficit.
Risk Factors
- Hypertension
- Hyperlipidaemia
- Smoking
- Diabetes
- Atrial fibrillation resulting in a cardiogenic embolus (remember, AF increases your clotting risk which is why it’s usually managed with anticoagulants)
- Oestrogen-containing medications such as the oral contraceptive pill as they leave you in a pro-thrombotic state
- Hypercoagulable states
- Patent foramen ovale: Right sided clots potentially passing into the left side circulation and embolising to the brain
- Carotid artery stenosis: Tends to result in unilateral embolic infarcts
Causes
- Thrombotic strokes
- Embolic strokes
- Hypotensive shock
- Arterial dissection
Clinical Features
To remember the main clinical features of strokes, you can think of the 4 main things the brain does, and work through it that way i.e. motor, sensory, cerebellar, and higher functions.
- Motor
- Hemiplegia: Unilateral paralysis
- Hemiparesis: Unilateral weakness
- Sensory: Sensory loss/reduction. Remember, sensation might not just be fine touch i.e. pressure, pain, and vibration can also be affected.
- Cerebellar Signs: DANISH signs (dysdiadokokinesia, ataxia, nystagmus, intention tremor, slurred speech, hypotonia)
- Higher Functions
- Apraxia: Difficulty in carrying out purposeful tasks e.g. being unable to draw a simple figure
- Dysphasia
- Receptive (Wernicke's): Speech is fluent, but will not make sense
- Expressive (Broca's): Speech is broken, but patients are able to comprehend speech and language
- Inattention/Neglect: An inability to perceive one side of space, contralateral to the side of the cerebral lesion. For example, the patient might only eat food on one side of the plate.
Ischaemic Stroke Syndromes
The precise clinical features of a stroke depend on which vascular territory the stroke has impacted. The Bamford classification system describes four main types:
- Total Anterior Circulation Stroke (TACS): Usually affects the Anterior Cerebral Artery + Middle Cerebral Artery
- Partial Anterior Circulation Stroke (PACS): Usually affects Anterior Cerebral Artery + Middle Cerebral Artery but to a lesser degree than a TACS
- Lacunar Syndrome: Usually affects the lenticulostriate/pontine/lacunar vessels
- Posterior Circulation Stroke (POCS): Usually affects Posterior Cerebral Artery/Vertebral/Basilar Arteries
- Total Anterior Circulation Stroke: All three of the following features must be present:
- Contralateral hemiparesis/hemiplegia/hemisensory loss of the face, arm and leg
- Contralateral homonymous hemianopia
- Disruption to higher cerebral function e.g.
- Dysphasia
- Apraxia
- Inattention/neglect
- Partial Anterior Circulation Stroke: Two of the three features of a total anterior circulation syndrome must be present OR disruption to a higher cerebral function alone
- Lacunar Stroke: This occurs when there is occlusion of the smaller lenticulostriate arteries. There is no loss of higher cerebral function such as dysphasia, and there is usually no hemianopia. You need one of the following:
- Motor disruption only
- Sensory disruption only
- Both sensorimotor disruption
- May have cerebellar signs
- Posterior Circulation Stroke: As this affects the posterior circulation, it mainly impacts the cerebellum, cranial nerve nuclei found in the brainstem, and the visual cortex which is found in the occipital lobe. Thus, it can produce the following symptoms:
- Cranial nerve palsy: For example, CN VII causing unilateral facial paralysis + a contralateral motor/sensory deficit
- Bilateral motor/sensory deficit
- Cerebellar dysfunction e.g. vertigo/nystagmus/ataxia
- Homonymous hemianopia/quadrantonopias
- No dysphasia or neglect
Ischaemic Stroke – Vessel Localisation
There are a lot of different stroke syndromes based on which vessel is affected, so we aren’t going to go through all of them but we’ll touch on the main ones:
Middle Cerebral Artery: This is the most commonly affected vessel, and supplies a large part of the brain.
- Contralateral weakness and sensory loss, usually worse in the face and upper limb
- Inattention if the non-dominant hemisphere affected (so usually seen in right hemisphere infarcts – even in left handed people, the right hemisphere is usually the dominant side)
- Dysphasia: Only seen in dominant hemisphere infarcts (so usually left infarcts) as that’s where the following two areas are:
- Wernicke’s: The area is supplied by the inferior part of the MCA. Results in a receptive dysphasia – speech is fluent, but it will not make sense.
- Broca’s: The area is supplied by the superior branch of the MCA. Results in an expressive dysphasia – speech is not fluent, but patient’s have in tact language comprehension.
- Contralateral superior quadrant visual field defect: Due to damage to the optic radiations
Anterior Cerebral Artery
- Contralateral weakness and sensory loss, usually worse in in the lower limbs
- Urinary incontinence
- Labile emotions
Posterior Cerebral Artery
- Contralateral homonymous hemianopia with sparing of the macula
- Double vision
- Nausea and vomiting
- Vertigo
- Memory loss
- Unilateral limb weakness
Differential Diagnosis
- Haemorrhagic stroke: For example, from a subarachnoid/subdural/extra or epidural haemorrhage
- Todd’s paresis: Occurs following a seizure
- Hypoglycaemia
- Bell’s palsy: Idiopathic cranial nerve VII palsy resulting in unilateral facial paralysis
- Cerebral abscess
- Brain tumour
ROSIER Tool
The ROSIER scale is a tool which can be used to differentiate between stroke and stroke mimics. Features such as loss of consciousness or seizures are more likely in mimics, weakening a diagnosis of stroke whilst features such as visual field defects or asymmetrical weakness make stroke more likely.
NIHSS Scale
The National Institute of Health Stroke Scale is a way of quantifying neurological deficit that arises secondary to a stroke. It measures various parameters including level of consciousness, eye movements, visual fields, facial palsy, motor function, sensory function, speech and language, ataxia, and inattention/neglect.
It is usually used to assess eligibility for treatments such as thrombectomy, and it can also be used to monitor response to treatment.
Investigations
Neuroimaging is a crucial component in stroke management as it dictates the management plan for patients. Thus, patients ideally should receive imaging within an hour of arrival at hospital. This is usually through CT to initially rule out haemorrhagic strokes (you don’t want to accidentally give a patient blood thinners thinking it’s an ischaemic stroke when it’s actually haemorrhagic).
If there is still diagnostic uncertainty after a CT head, MRI can be used (usually diffusion weighted imaging).
Bedside
- ECG: Looking for atrial fibrillation
- Blood glucose: Hypoglycaemia can be a stroke mimic, and hyperglycaemia is sometimes seen in intracranial haemorrhage
- Scoring Systems: NIHSS and ROSIER
- Neurological Examination
- Tone: Initially flaccid, but ultimately spasticity will develop
- Power: Reduced power
- Coordination: You may see ataxia/nystagmus/dysdiadokokinesia
- Reflexes: Hyperreflexia due to an upper motor neuron lesion
- Sensation: Reduced
Bloods
- FBC, U&E, LFT, CRP: Baseline
- Cholesterol and HbA1c: To ascertain risk factors
- Clotting screen: Any clotting abnormalities
Imaging
- CT Head: Imaging modality of choice to rule out a haemorrhage. Ischaemic strokes appear dark i.e. with low attenuation on a CT but they aren’t always seen immediately
- MRI: Usually done when there’s diagnostic uncertainty. It’ll allow visualisation of the cytotoxic/vasogenic oedema that we talked about in the pathophysiology section. Diffusion-weighted MRIs tend to be used in earlier stages as it's more sensitive and specific.
- Doppler ultrasound of carotid arteries: Looking for carotid stenosis, particularly important for patients with a stroke in the carotid territory i.e. anterior circulation
Management
General
- Any patients acutely unwell/low GCS need to be managed in an A-E manner (Airway, Breathing, Circulation, Disability and Exposure)
- If available, patients need to be admitted to hyperacute stroke units (HASU) within 4 hours of presenting.
- Assess swallow before oral intake as patients can have dysphagia and therefore an unsafe swallow.
Definitive
So, we know an ischaemic stroke occurs due to a sudden lack of blood supply resulting in tissue death. The aim of treatment is to restore that blood supply and salvage as much brain tissue as possible, and this is done by removing the clot. Now you can either remove the clot with drugs, or you can do it mechanically by physically extracting the clot – this is thrombolysis and thrombectomy respectively.
Thrombolysis:
- Alteplase: This is a tissue plasminogen activator. Plasminogen is a precursor to plasmin which is an enzyme that breaks up fibrin and fibrinogen i.e. the components of clots – it essentially dissolves clots.
- Needs to be given within 4.5 hours of stroke onset + intracranial haemorrhage has been ruled out.
- Thrombolysis is not without complications so after its delivery, patients need to be monitored carefully – a big one, is patients developing intracranial haemorrhages after treatment.
- You want to be careful with thrombolysis as there are contraindications and based on how it works, they’re usually related to bleeding e.g.
- History of intracranial haemorrhages
- Known intracranial neoplasm
- Concurrent anticoagulation
- Bleeding disorder
- Recent surgery
- Recent GI/GU bleed
Mechanical Thrombectomy: This involves mechanical extraction of a clot for ischaemic stroke. NICE recommend that this be offered:
- Within 6 hours of symptom onset
- Alongside IV thrombolysis (provided it isn’t contraindicated and you’re still within the 4.5 hour time window)
- Only if a magnetic resonance angiogram or CT angiogram has shown an occlusion in the proximal anterior circulation
- There are other instances this can be offered but we won’t delve into them for sake of simplicity – if you’re interested, it’s 1.4.6 and 1.4.7 on the NICE guideline for stroke.
Aspirin:
- A 300mg STAT dose is given within 24 hours of symptom onset and continued at that dose for 2 weeks, after which longer term anticoagulation is initiated (unless the patient has been thrombolysed, in which case you usually wait 24 hours to initiate aspirin after thrombolysis, due to the risk of haemorrhagic transformation).
- This can be given orally if the patient does not have dysphagia – otherwise, it should be given rectally or through an enteral tube.
- A proton pump inhibitor can also be given in conjunction to prevent dyspepsia.
Secondary Prevention and Information for After a Stroke
- Treat modifiable risk factors: Smoking cessation, manage hypertension, keep alcohol intake within 14 units/week etc.
- Statins to control hyperlipidaemia
- Antiplatelets: Patients will usually require 75mg clopidogrel daily. If a patient cannot have clopidogrel, aspirin 75mg with modified release dipyridamole 200mg can be used.
- Anticoagulation: In patients where AF was thought to be the cause of the stroke, anticoagulation in the form of DOACs or warfarin is usually started 2 weeks after the stroke
- Patients should not drive for 1 month after a stroke, but they don’t need to tell the DVLA unless there is persistent neurological deficit after 1 month
- Neurorehabilitation: Comprises of an MDT approach of people such as nurses, dietitians, physiotherapists, occupational therapists, speech and language therapists etc.
- Carotid endarterectomy: For patients with >50% carotid artery stenosis
Complications
- Depression
- Pain following a stroke: Particularly headaches
- Seizures
- Hydrocephalus
- Aspiration pneumonia: From poor swallow
- Elevated intracranial pressure +/- brain herniation
- Haemorrhagic transformation
References
https://www.ninds.nih.gov/disorders/all-disorders/apraxia-information-page
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4602245/
https://www.strokeaudit.org/SupportFiles/Documents/Guidelines/2016-National-Clinical-Guideline-for-Stroke-5t-(1).aspx
https://patient.info/doctor/thrombolytic-treatment-of-acute-ischaemic-stroke#nav-4
https://calgaryguide.ucalgary.ca/ischemic-stroke-pathogenesis/
https://www.thieme-connect.com/products/ejournals/pdf/10.1055/s-0040-1721165.pdf