Cholangitis, acute cholangitis, or ascending cholangitis refers to a severe infection of the biliary tree.
Pathophysiology
- The underlying mechanism of acute cholangitis is due to bile stasis.
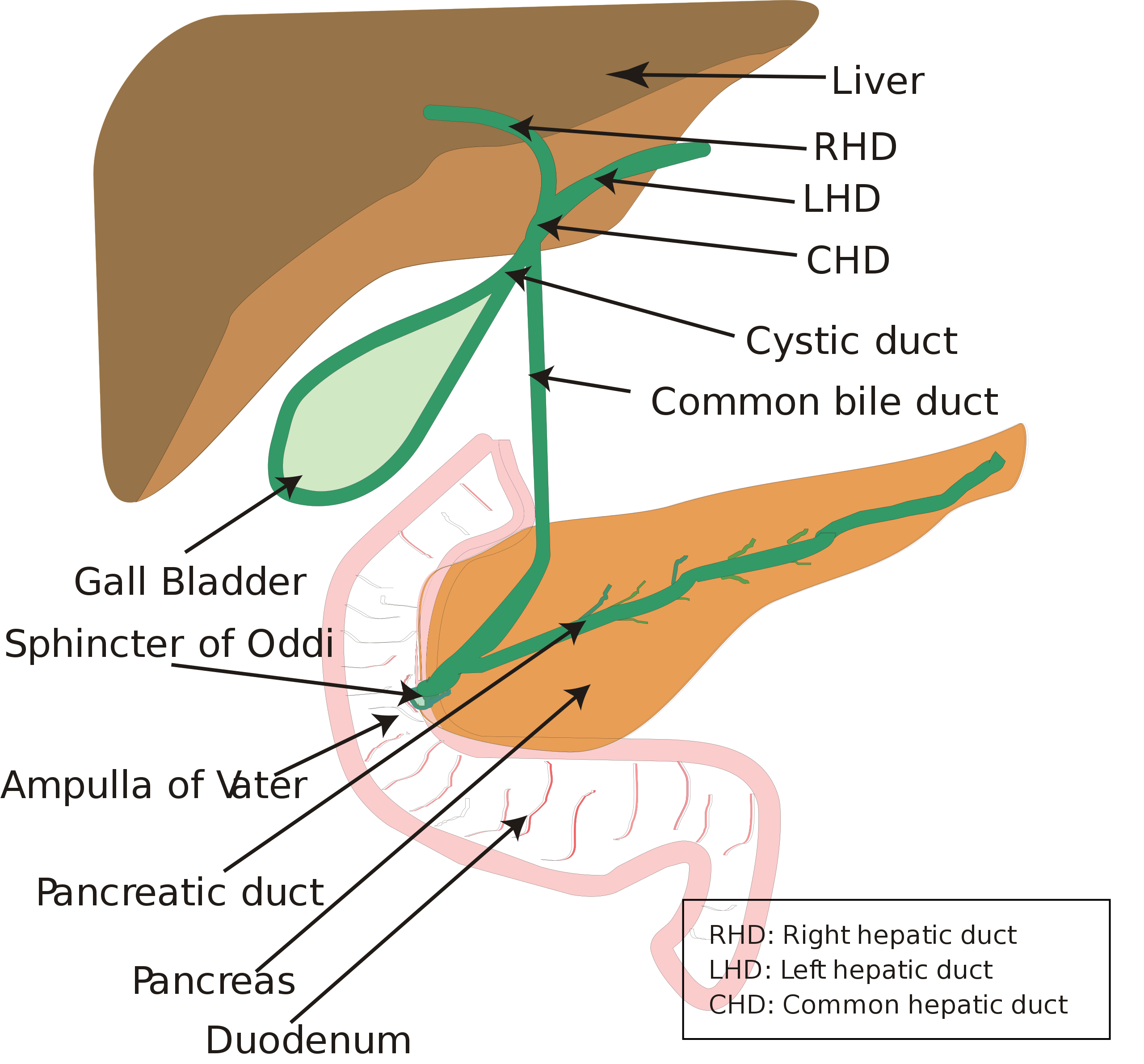
- It is possible for bacteria to ascend from the duodenum, through the ampulla of Vater and into the biliary tree. However, protective mechanisms exist to prevent this happening e.g. the sphincter of Oddi and continuous flow of bile.
- Biliary mucus and secretory IgA also prevent the adherence of bacteria to the biliary tree, further preventing bacterial colonisation and infection in the biliary system.
- If there is an obstruction e.g. a stone in the common bile duct (CBD), or biliary strictures, it raises the pressures within the biliary tree causing the protective antimicrobial mechanisms to fail, thus putting the patient at risk of an infection of the biliary tree – acute cholangitis.
- The most common causative bacteria are typically gram-negative bacilli e.g. E.coli, Klebsiella and Enterobacter.
- Due to the obstruction, pressure in the biliary tree builds which increases the chances of bacterial translocation into the blood – this results in sepsis.
Biliary_system.svg: Vishnu2011derivative work: Vishnu2011, Public domain, via Wikimedia Commons
Biliary Tree Diagram
Causes
- Choledocholithiasis: CBD stones
- Biliary duct strictures
- Tapeworm/Roundworm
- Malignancy: Pancreatic/Gallbladder etc
Clinical Features
- Charcot’s triad:
- Fever
- RUQ Pain
- Jaundice: Acute cholangitis is most often associated with an obstruction, so patients can develop obstructive jaundice with yellow skin, sclera, and mucous membranes
- Reynold's pentad: Charcot’s triad + hypotension and confusion. Seen in more severe cases
- Pruritis: Due to bile salts not being cleared by entering the gut. They cause itching.
- Pale stools: Excess levels of conjugated bilirubin which cannot reach to gut to be converted into urobilinogen and then stercobilin which is what colours faeces brown
- Dark urine: Excess conjugated bilirubin turns urine dark
Differential Diagnosis
- Cholecystitis
- Pancreatitis
- Acute Hepatitis
- Biliary Colic
Investigations
Bloods
- Full blood count: Looking for raised white cells
- U&Es: Baseline
- LFTs: May show cholestatic picture with raised ALP and gGT. Transaminases and bilirubin may also be raised
- CRP: Inflammatory marker
- Blood cultures
- VBG: May be indicated if sepsis is suspected as patient may be at risk of a metabolic acidosis secondary to high levels of lactate
- Clotting screen/INR: Raised INR may suggest hepatic dysfunction
Imaging
- Abdominal ultrasound is the usual first line investigation
- Magnetic resonance cholangiopancreatography (MRCP): If ultrasound is negative
Management
General
- IVF – fluid resuscitation if patients are in septic shock
- Analgesia
- IV Antibiotics
- Sepsis screen: Blood cultures, urine cultures etc
- Considering ITU/HDU if required
Biliary Drainage
- Endoscopic retrograde cholangiopancreatography (ERCP): This is the preferred method of relieving the biliary obstruction and enabling decompression
- A procedure that combines endoscopy and x-ray technology
- Similar to an OGD in that the endoscope is passed from mouth, down oesophagus, into the stomach, and then into the duodenum to enter the biliary tree
- Once in the biliary tree, obstructions can be relieved e.g. stones can be removed, strictures can be stented, the sphincter of Oddi can be incised to make it larger and easier for CBD stones to pass etc.
- Endoscopic ultrasound (EUS) guided drainage
- Percutaneous transhepatic cholangiography (PTC)
- Accessing the biliary tree via needle through the skin, into the liver, and then through to the biliary tree.
- This usually is done when ERCP cannot be performed
- Open surgical drainage
Management of Common Bile Duct Stones
Stones which are lodged in the common bile duct require clearance alongside a laparoscopic cholecystectomy, regardless of whether or not they are causing symptoms in accordance with NICE guidance.
Complications
- Hepatic abscess
- Acute pancreatitis
References
https://www.ncbi.nlm.nih.gov/books/NBK558946/
http://www.emergencymedicalparamedic.com/what-is-renolds-pentad/
Netter’s Integrated Review of Medicine
https://www.macmillan.org.uk/cancer-information-and-support/diagnostic-tests/percutaneous-transhepatic-cholangiogram-ptc