An abdominal aortic aneurysm (AAA) describes a swelling in the wall of the abdominal aorta. A rupture and subsequent bleed of an AAA is a medical emergency.
Risk Factors
- Smoking
- Increasing age
- Caucasian race
- Male (Although women are more likely to rupture an AAA)
- Family history
- Hyperlipidaemia
- Hypertension
- Peripheral vascular disease
Clinical Features
Many AAAs are incidental findings e.g. an abdominal ultrasound may be done for another different clinical indication and incidentally, a AAA is found on the ultrasound. It could also present incidentally due to an abdominal examination which will reveal an expansile, pulsatile and non-tender abdominal mass (hence the importance of palpating the abdominal aorta as part of an abdominal examination).
Alternatively, it may present as a ruptured aneurysm in which case the patient will likely have the following:
- Haemodynamic instability
- Cardiogenic shock i.e. syncope, pre-syncope, cold peripheries, reduced capillary refill time, hypotension, tachycardia, feeling clammy/sweaty
- Abdominal pain which radiates to the back
- Back pain
- Loin pain
- Spots of ischaemia in the distal limbs secondary to emboli breaking off from the aneurysm
- Aortocaval fistula: This is a very rare complication of an AAA and occurs when the aneurysm erodes and then ruptures into the inferior vena cava which can cause confusing signs and symptoms. Such a fistula would result in higher venous pressures which may cause heart failure or pulmonary congestion.
Differential Diagnosis
- Renal colic
- Peptic ulcer
- Acute pancreatitis
- Myocardial infarction
- Musculoskeletal back pain
Investigations
Bedside
- Urinalysis: To check for haematuria for signs of renal stones or pyelonephritis
- Observations: Particularly blood pressure and heart rate to look for signs of hypovolaemic shock
Bloods
- FBC, U&E, LFT, Clotting screen: Baseline
- G&S and XM: If the patient does have a ruptured AAA, they will require a blood transfusion
Imaging
- Abdominal ultrasound: Sensitive and specific for AAAs and are useful for screening. In the UK, there is an active screening programme for AAA which is offered to men the year they turn 65. This is done as a one off i.e. if the scan is normal, further ultrasounds are not repeated. If an AAA is found, subsequent surveillance ultrasounds are performed.
- 3-4.4cm: Follow-up scan in 1 year
- 4.5-5.4cm: Follow-up scan in 3 months
- >5.5cm: Consider surgery
- CT angiogram: Can give a more precise measurement for the size of the aneurysm and is the choice modality for a symptomatic AAA. A CT also enables identification of other involved vessels e.g. the common iliac arteries.
- Magnetic resonance angiogram (MRA): Can be used if the patient is allergic to IV contrast.
Management
Asymptomatic AAAs are usually not operated on until they reach around 5.5cm. This is due to the risk of rupture being low for smaller aneurysms i.e. the 5-year rupture rate for asymptomatic AAAs <4cm is nearly 0%, but this rises to 25-40% for aneurysms >5cm.
NICE specify three situations in which to consider repair unruptured AAAs:
- Symptomatic AAAs
- Asymptomatic, >4cm and growing by more than 1cm in a year
- Asymptomatic, >5.5cm
There are two main techniques through which AAAs can be repaired – either through:
- Open surgical repair: The aneurysm is exposed and clamped proximally and distally. The aneurysm is then replaced by a prosthetic graft. Open surgery is recommended by NICE for elective repair of AAA, unless there are medical co-morbidities or other abdominal pathologies such as a horseshoe kidney or stoma, in which case endovascular aneurysm repair may be more appropriate.
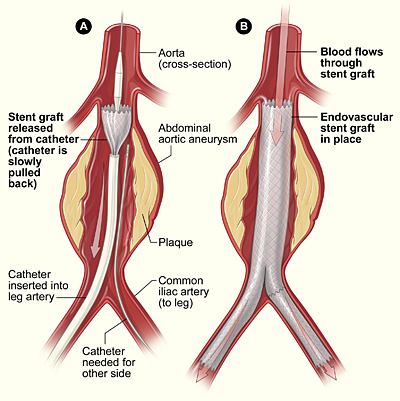
- Endovascular aneurysm repair (EVAR): Rather than surgically exposing the aorta, a graft is introduced within the vessel. This allows blood to flow through the graft and the surrounding aneurysm to thrombose.
Risk factors should also be managed. This includes:
- Blood pressure control
- Smoking cessation: reduces the risk of AAA rupture, so individuals should be offered smoking cessation advice.
- Statin therapy
- Diabetes management
By National Institutes of Health - http://www.nhlbi.nih.gov/health/dci/Diseases/arm/arm_treatments.html, Public Domain, https://commons.wikimedia.org/w/index.php?curid=12837854
Endovascular Repair of Aneurysm
Emergency Management
Patients require management for their shock e.g. through activation of the Major Haemorrhage Pathway. A group and save + rapid crossmatch will be necessary alongside baseline bloods.
Definitive management is again with surgical repair. As per NICE guidelines, for ruptured aneurysms, EVAR generally provides more benefit for men over 70 or women of any age, whilst open surgery provides a better balance of benefit and harm for men under 70.
DVLA
- Bus, coach and lorry drivers: Any size aneurysm must be reported to the DVLA. >5.5cm aneurysm, license will be suspended until aneurysm is treated.
- Car drivers: 6cm aneurysm, must inform DVLA. License will be suspended at 6.5cm, until aneurysm is treated.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4863798/
https://www.nice.org.uk/guidance/ng156/chapter/Recommendations#diagnosis
Ferri’s Clinical Advisor 2021 Abdominal Aortic Aneurysm
https://patient.info/doctor/abdominal-aortic-aneurysms#nav-0
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/598365/AAA_Screening_Standard_Operating_Procedures_March_2017.pdf
https://www.gov.uk/aneurysm-and-driving
https://www.gov.uk/government/publications/monitoring-your-medium-abdominal-aortic-aneurysm/your-screening-results-you-have-a-medium-abdominal-aortic-aneurysm-aaa#driving