Multiple sclerosis (MS) is an autoimmune disease characterised by the destruction of the myelin sheath which surrounds nerves. It is a chronic disease though patients may experience periods of remission as well as flare-ups, the latter of which manifests with neurological symptoms.
Epidemiology
It is estimated that there are just over 2 million cases of multiple sclerosis globally as of 2016. The condition tends to affect women twice as much as men. The disease will present in fairly young age, between the ages of 20 and 40.
Causes
The cause of MS is thought to be a combination of environmental and genetic factors, with people exhibiting a positive family history having an increased risk of developing MS. Several genes have also been identified which seem to increase the risk of developing MS. Though there is uncertainty as to which environmental factors can lead to MS, theories include exposure to Epstein-Barr virus in genetically susceptible individuals can lead to development of the disease.
Pathophysiology
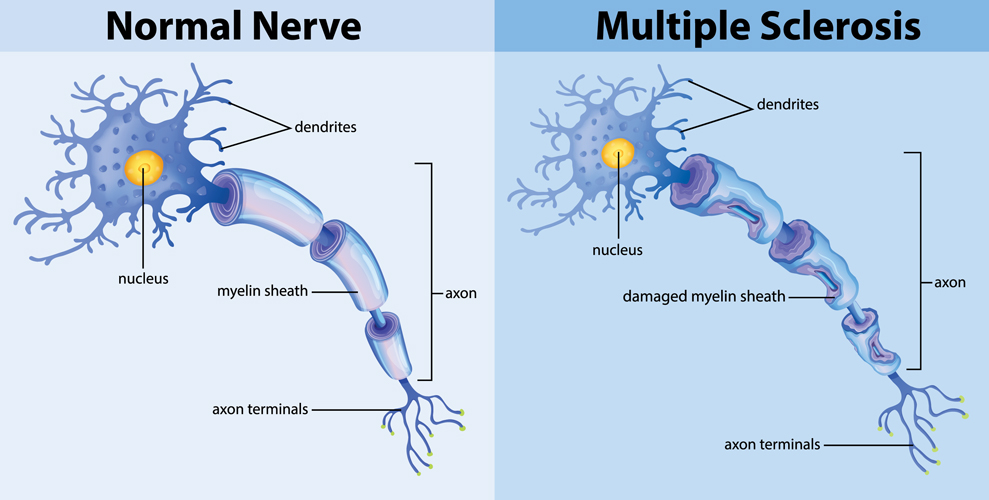
- The pathophysiology of MS is quite complex, but it is thought to mainly involve T cells, although other immune cells also have a role.
- One proposed theory suggests antigen presenting cells activate T cells, causing them to express adhesion molecules that allow the T cells to cross the blood-brain barrier – something they would otherwise be unable to cross. Once the T cells enter into the central nervous system, they start to release cytokines.
- This recruits more inflammatory cells including B cells which can now produce antibodies against the myelin sheath of neurones. Ultimately, this leads to destruction of the myelin sheath.
- This can manifest itself as a flare up of symptoms.
- The body does try to repair this destruction by remyelinating axons and this manifests clinically as an improvement in symptoms.
- Over time however, the repeated demyelination and remyelination cycle will lead to permanent scarring at multiple sites across the central nervous system – hence the name “multiple sclerosis”. The sites of demyelination are also known as plaques.
Copyright Medic in a Minute 2023
Nerve in Multiple Sclerosis
Now that you know the pathophysiology, you can understand why MS is regarded as both a neuroinflammatory process due to inflammatory immune cells being involved, as well as a neurodegenerative process due to gradual deterioration of the myelin sheaths in the central nervous system.
Clinical Features
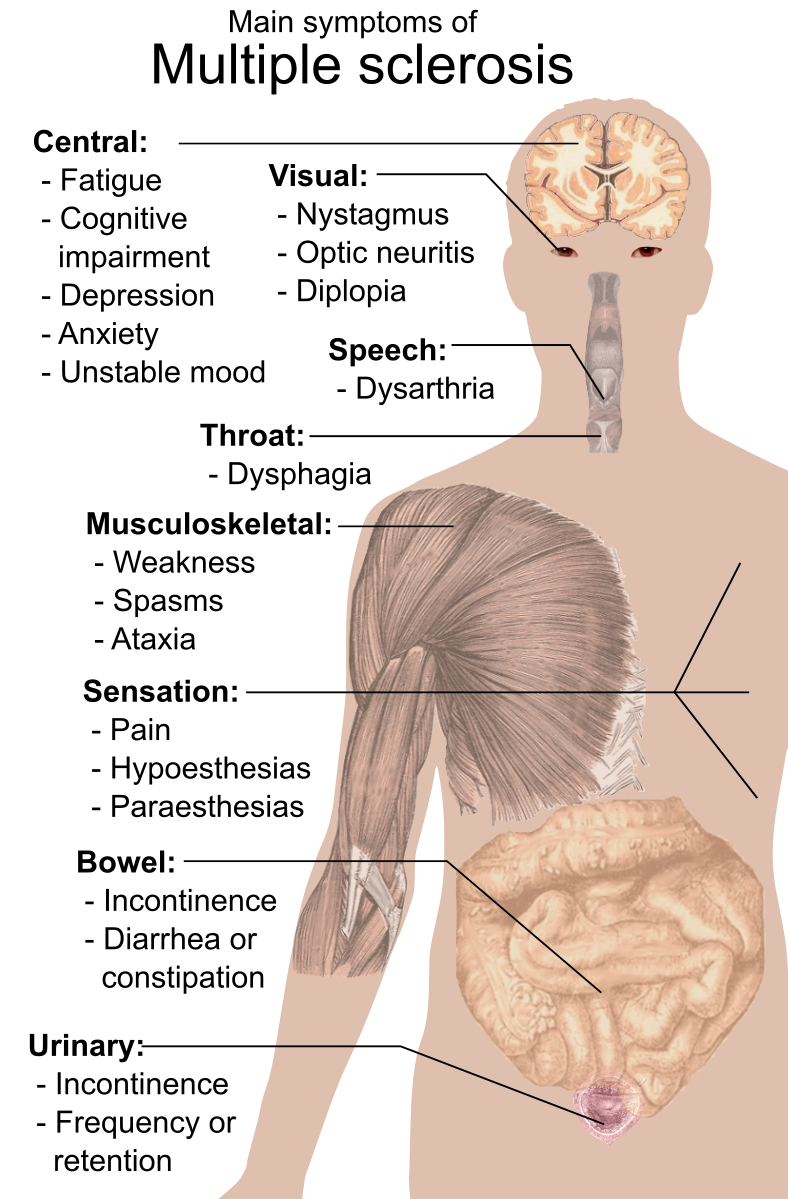
The symptoms of multiple sclerosis depend on which part of the central nervous system is demyelinating. For example, if you have plaques all over the cerebellum, your patient may have cerebellar symptoms such as ataxia, dysarthria and nystagmus. If there are plaques along the optic nerve, the patient may experience visual symptoms.
The easiest way to think of symptoms is to consider the nervous system, followed by what symptoms occur when something goes wrong with each part. For example:
- Sensory:
- Paraesthesia in odd patches
- Numbness
- Loss of vibration/proprioception
- Motor:
- Cerebellum:
- Ataxia
- Dysarthria
- Nystagmus
- Intention tremor
- Autonomic:
- Sexual dysfunction
- Bladder/bowel dysfunction
- Ocular:
- Optic Neuritis: Optic neuritis is when the optic nerve becomes inflamed as a result of the demyelination.
- Patients may present with eye pain, vision loss, pain on eye movements and colour changes whereby colours may appear ‘washed out’. Red colour vision is particularly affected.
- Optic papillitis: Head of the optic nerve is inflamed, and this is visible on ophthalmoscopy.
- Retrobulbar neuritis: When the optic nerve is inflamed prior to entering the eye.
- General:
Mikael Häggström, Public domain, via Wikimedia Commons
Symptoms of Multiple Sclerosis
Specific Signs
- Charcot’s Neurological Triad: This is a triad of symptoms – dysarthria, nystagmus and an intention tremor suggest the presence of multiple sclerosis.
- Uhtoff’s phenomenon: Symptoms worsen on exposure to heat. So a patient describing worsened symptoms after exercising may prompt further investigations to look for MS.
- L’hermitte’s sign: This is when flexion of the neck leads to a sudden, electric-shock like pain that shoots down the spine and radiates out into the limbs.
Types
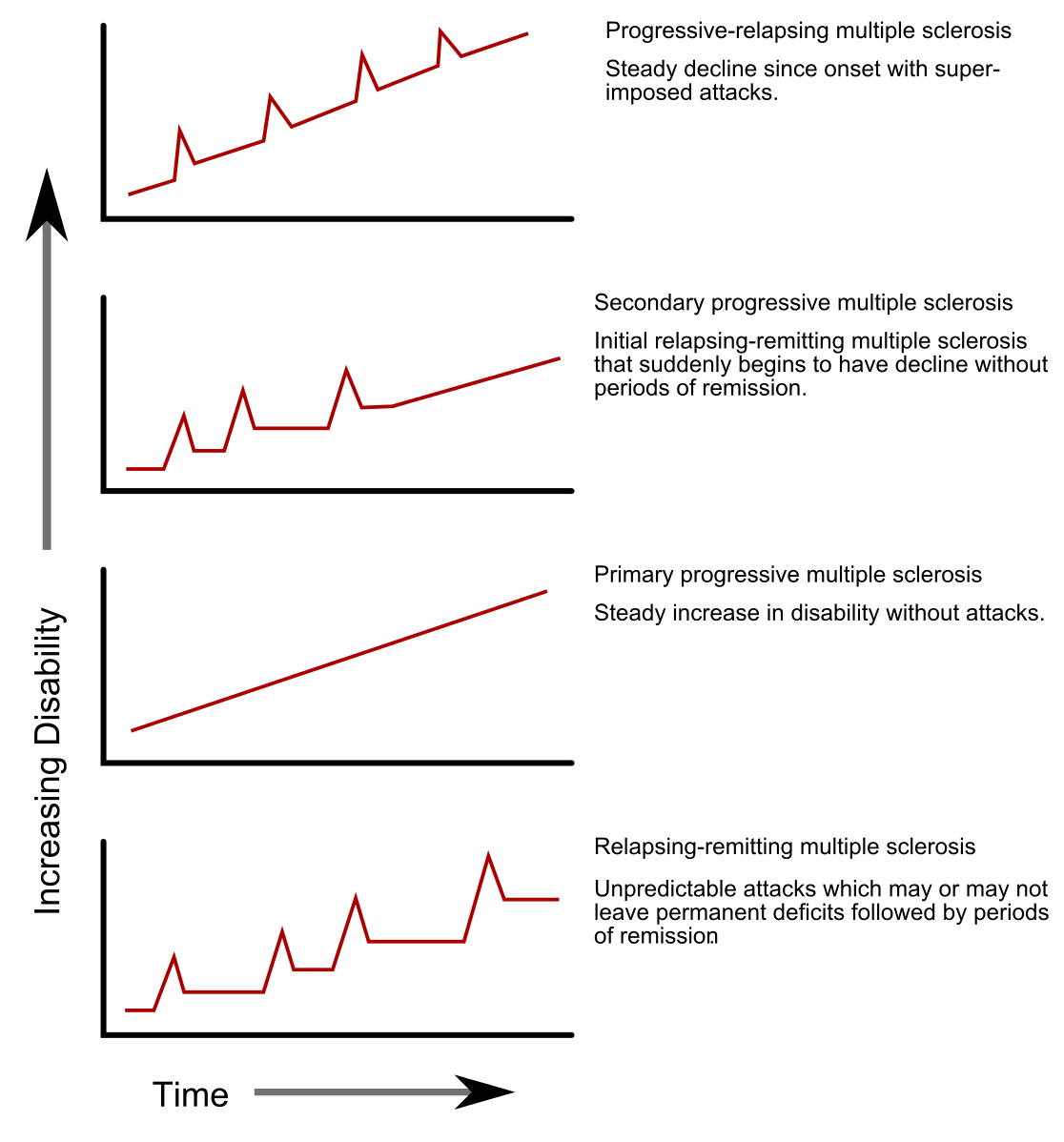
There are four patterns that MS tends to follow.
Relapsing-Remitting
- This is the most common type.
- Patients experience symptomatic flare up periods (the relapses) which last a few days. This correlates to periods of demyelination.
- They then start to recover as oligodendrocytes, cells which produce myelin, start to remyelinate axons. This takes a few weeks and ultimately, patients may either partially or completely recover.
- If patients are only partially recovering after every flare up, after enough time passes there will be marked disability compared to when their function when the disease process first started.
Primary Progressive
- This is where patients do not have relapses or remissions – the disease is simply progressively getting worse and worse, with subsequent increase in disability.
Secondary Progressive
- These are patients who start off as relapsing-remitting but then develop into a progressive pattern whereby the disability is steadily increasing without any clear flare ups or remissions.
- Many patients of the relapsing-remitting type will progress to develop this pattern of disease.
Relapsing-Progressive
- This is the least common pattern.
- Patients essentially have primary progressive MS whereby disability steadily increases.
- In addition to this, they have superimposed flare ups or relapses leading to rapidly progressing disability.
GetThePapersGetThePapers at English Wikipedia, Public domain, via Wikimedia Commons
Types of Progression in Multiple Sclerosis
Investigations
MRI
MRI is a key diagnostic tool for identifying MS. Depending on the type of the MRI, the appearance may vary. For example:
- T1 Weighted: Fat appears bright in this scan. We know myelin is quite fatty so loss of myelin will have low attenuation i.e. areas of lost myelin will look like black holes.
- T1 Weighted + Gadolinium: Gadolinium contrast causes breakdown of the blood-brain barrier to become highly attenuated (bright) and signifies active breakdown. Thus you see a ring of high attenuation surrounding the ‘black holes’ where the myelin has been lost.
- T2 Weighted: Fluid appears bright in this scan. Since plaques are inflammatory lesions, you would expect to find fluid as part of an inflammatory process, hence you will see areas of high attenuation.
CSF
- A lumbar puncture can be performed to look for oligoclonal bands in the CSF.
- Presence of these would suggest there is an active inflammatory process going on which is restricted to the central nervous system.
Evoked Potentials
- This is a method of measuring the speed of conduction by the nerves.
- You can measure sensory evoked potentials, auditory evoked potentials or visual evoked potentials.
- Since myelin acts as an insulator, you would expect nerves which have lost their myelin sheaths to transmit nervous impulses slower. The speed of conduction is reduced and this can help strengthen the diagnosis of MS.
Management
Conservative
- Exercise
- Smoking cessation
- CBT
- Vestibular Rehabilitation: Can be used for individuals with mobility issues related to standing balance
Medical
- Fatigue:
- Spasticity: Patients can get muscle spasms, stiffness and pain
Acute Relapses
- Usually treated with oral methylprednisolone, or potentially IV for people with severe relapses.
Disease-Modifying Therapies
- Beta-interferon: These are usually used as first-line treatments in MS. They are thought to work by reducing inflammation and suppressing immune responses.
- Glatiramer acetate: Sometimes used first-line as well – works my modulating the effect of immune cells against myelin.
- Dimethyl fumurate: Works by decreasing inflammation as well
- Fingolomid: A drug which sequests immune cells in lymph nodes to prevent them causing inflammation in the CNS
- Monoclonal antibodies such as Natalizumab an Alemtuzumab act against T cells to try and stop the inflammatory process. Other drugs include dimethylfumurate and beta-interferon.
References
https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(18)30443-5/fulltext
https://u.osu.edu/multiplesclerosis/pathophysiology-and-clinical-presentation-correct-diagnosis/
Kumar and Clark's Clinical Medicine, Tenth Edition