A myocardial infarction (MI), or heart attack, occurs when ischaemia to the heart tissue results in myocardial necrosis.
Pathophysiology
The most common cause of an MI is atherosclerosis. Atherosclerosis is a condition where fat builds up inside the walls of arteries.
- Atherosclerosis begins as a fatty streak, which is simply a streak of lipid-laden macrophages in the intima of the arterial vessel. Macrophages attempt to phagocytose away the lipid, and thus become lipid-laden and foamy in appearance (and can therefore be referred to as foamy macrophages).
- Low-density lipoproteins (LDL) are a major culprit in further development of atherosclerosis, as lipid accumulation in the walls of blood vessels tends to occur when there are increased levels of LDLs.
- As lipid continuously accumulates in the vessel wall and foam cells, there is recruitment of smooth muscle cells and fibroblasts which secrete an extracellular matrix. This is where the fatty streak begins to evolve into an atherosclerotic plaque.
- These plaques begin to stenose part of the vascular lumen, potentially causing ischaemia. This is where patients can begin to develop signs such as angina pectoris or transient ischaemic attacks, depending on if the stenosis is occuring in coronary vessels or cerebral vessels respectively.
- At the core of the atherosclerotic plaque is necrotic material due to dead macrophages and foam cells. With time, some of these plaques can become completely fibrotic and are thus known as fibrous plaques. Others can form a thin fibrous cap only on top of the plaque.
- Fibrous plaques are fairly stable, but unstable plaques that have thinner fibrous caps are concerning. If the cap ruptures, a thrombus will form on top of the atherosclerotic plaque which will further reduce the size of the lumen – this is what can result in a myocardial infarction if it were to occur in a coronary artery.
- There are two major responses of the body in case of an MI. Firstly, the sudden disruption to the cardiac tissue results in a drop in cardiac output, meaning the end diastolic volume is higher (less blood leaving the heart, more blood hanging around inside the heart). This stretches the heart, which, via the Frank-Starling mechanism will result in increased contractility. This attempts to maintain cardiac output, but it cannot do so for long. Thus, the body activates the sympathetic nervous system to maintain cardiac output.
- The drop in cardiac output also results in a decreased blood pressure, thus activating baroreceptors and in turn, the sympathetic nervous system which tries to maintain cardiac output and blood pressure.
Causes
Although atherosclerosis is the most common cause of an MI, other causes include coronary vasospasm, coronary artery dissection, trauma, cocaine and coronary artery emboli.
Risk Factors
Can be split into modifiable e.g. smoking, diabetes mellitus, sedentary lifestyle, obesity, hyperlipidaemia, hypertension etc, and non-modifiable which includes being male, family history and age.
Clinical Features
Chest pain is of course the major symptom of an MI, but in elderly patients or those with diabetes, silent MIs are possible i.e. those which do not cause chest pain.
- Chest pain at rest: Can be describes as a crushing/tightness/intense pressure/heaviness
- Dyspnoea
- Nausea and/or vomiting
- Diaphoresis and/or pallor due to activation of the sympathetic nervous system
- Anxiety or ‘feeling of impending doom’
- Syncope: Usually due to profound hypotension or an arrhythmia
- Sudden death: From ventricular fibrillation or asystole
Investigations
Bedside
- History and examination
- ECG: ECG is the mainstay of diagnosis as it allows confirmation of an MI. There are two types of MI – one with ST segment elevation (STEMI) or a non-ST segment elevation (NSTEMI).
- STEMI features: Either persistent ST segment elevation or a new left bundle branch block
- NSTEMI features: ST depression or T wave inversion/flattening
- General features: After a few hours/days, pathological Q waves can develop and persist on the ECG. T waves may also become inverted and persist on the ECG, indicating the patient has a history of myocardial infarction.
Bloods
- FBC, U&E, LFT, TFT: Baseline
- HbA1c, Lipid Profile: Assess risk factors
- Cardiac Markers
- Troponin T and I: Specific cardiac muscle enzymes which leak out of cells if there is necrosis of the myocardium. This is helpful to differentiate from unstable angina (UA) – in UA, tissue doesn’t die so troponin does not rise. These are usually measured as serial troponins i.e. when the patient presents, then a few hours later. A troponin rise would be suggestive of myocardial infarction.
- Creatinine kinase: The first to rise alongside troponin T and I
- Aspartate aminotransferase (AST): Rises after creatinine kinase
- Lactate dehydrogenase: Rises last
- ESR/CRP: Elevated
Imaging
- Echocardiogram: To look for regional wall motion abnormalities or assess ventricular function following MI
- Chest x-ray: Look for pulmonary oedema, cardiomegaly and rule out other differentials
- CT/MRI coronary angiography: Look for evidence of cardiovascular disease
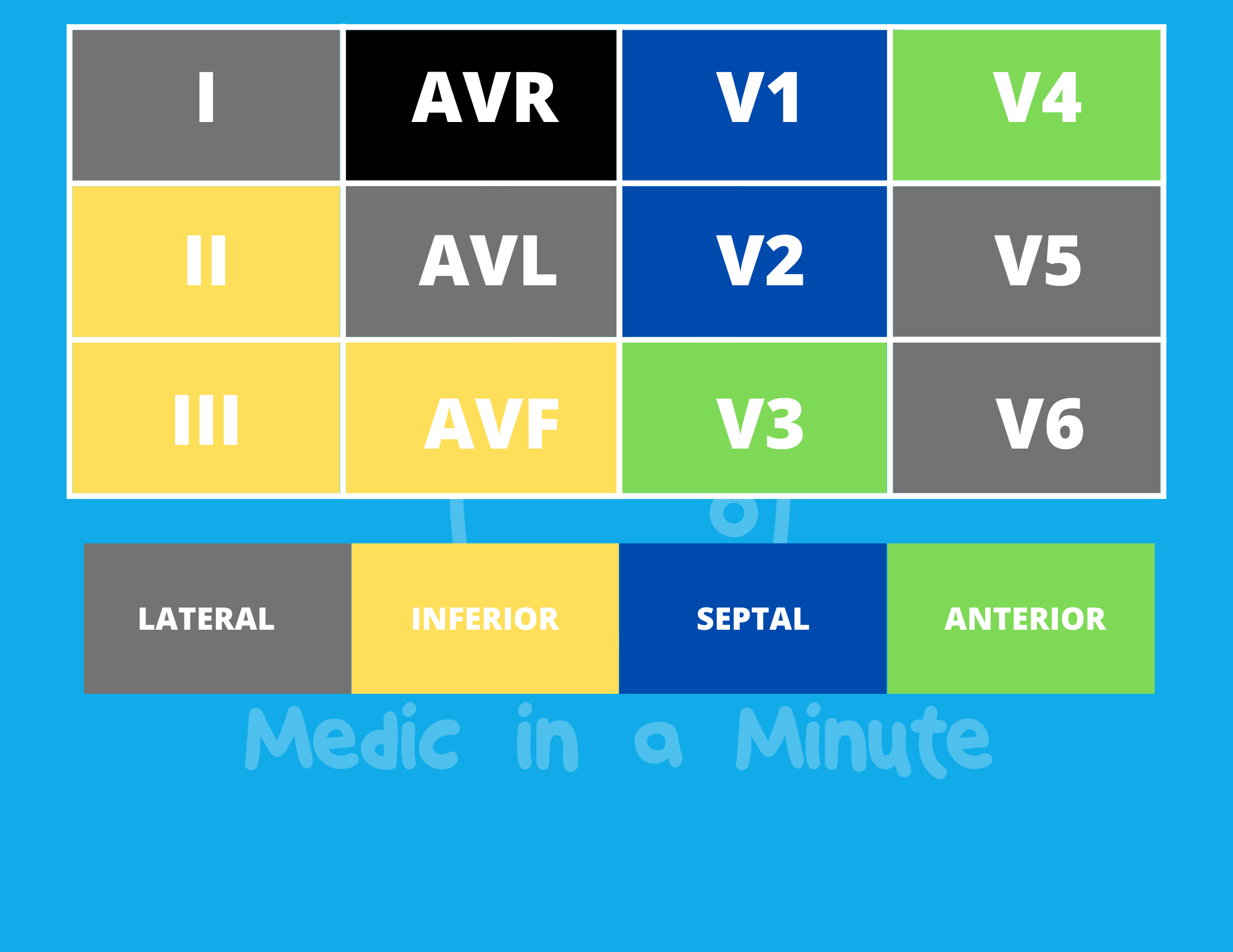
ECG and Locality of the MI
Copyright Medic in a Minute 2022
Localising an MI on ECG
General Management
Management of STEMIs and NSTEMIs are slightly different, so we will discuss each in turn. Initial therapy for a myocardial infarction however should include:
- Analgesia: Pain relief usually with nitrates e.g. sublingual glyceryl trinitrate (GTN) and/or opiates such as morphine or diamorphine. If prescribing morphine, it’s worth co-prescribing an anti-emetic such as ondansetron or metoclopramide as a side effect of opiates is nausea.
- Dual antiplatelet therapy: 300mg Aspirin + an ADP receptor antagonist e.g. clopidogrel, prasugrel or ticagrelor.
- Oxygen: Oxygen use is controversial - some sources state it can be harmful to administer oxygen if the patient is not hypoxic so local protocols surrounding oxygen administration should be followed. Generally speaking, oxygen is offered if patients have an oxygen saturation <94%, or to patients with COPD and are at risk of hypercapnic respiratory failure – in these patients, a saturation of 88-92% is the target.
Reperfusion Therapy
‘Time is tissue’ i.e. you want to restore perfusion to the myocardium as soon as possible to salvage cardiac tissue – this is known as reperfusion therapy. There are two main reperfusion strategies:
- Percutaneous coronary intervention (PCI): Involves passing a catheter into the coronary artery and inflating a balloon which expands the coronary artery – this is known as an angioplasty. Following this, the coronary is typically stented to keep the coronary artery open. A PCI is just an angioplasty + stenting of the vessel.
- Fibrinolysis: Same as thrombolysis or plasminogen activators. These drugs help to lyse the blood clot, thus relieving the obstruction. There are three main drugs used for fibrinolysis:
- Tissue plasminogen activator (tPA) e.g. Alteplase, tenecteplase
- Streptokinase
- Urokinase
STEMI Management
The following summarises the NICE guidance for the acute management of STEMIs.
- Primary PCI is offered if:
- Patients present within 12 hours of symptom onset AND PCI can be given within 120 minutes of the time frame in which fibrinolysis could have been given
- PCI can also be considered in those who are presenting after 12 hours of symptom onset but have ongoing myocardial ischaemia/cardiogenic shock
Dual Antiplatelets and PCI
If a patient is going to undergo PCI, they require dual anti-platelet therpay.
- No previous oral anticoagulation: Prasugrel + Aspirin
- Already on oral anticoagulation: Clopidogrel + Aspirin
Antithrombin Therapy with PCI
PCI patients also receive antithrombin therapy during the procedure. NICE recommend the following:
- PCI via Radial Artery: Unfractionated heparin with a bailout glycoprotein IIb/IIIa inhibitor
- PCI via Femoral Artery: Bivalirudin can be considered alongside a bailout glycoprotein IIb/IIIa inhibitor.
Bailout glycoprotein IIb/IIIa: This is where the drug is used as a ‘bailout’ i.e. the clinician did not initially intend to use the drug but throughout the PCI, it may be beneficial to give this drug.
Multivessel Revascularisation
If multiple coronary vessels are diseased, multivessel revascularisation can be performed provided the patient is not in cardiogenic shock – if they are, culprit vessel revascularisation is typically prioritised.
- Fibrinolysis
- Patients presenting within 12 hours of symptom onset, where PCI can’t be given within 120 minutes of symptom onset are usually offered fibrinolysis.
- Fibrinolysis is also offered to those who have presented more than 12 hours after symptom onset. An anti-thrombin is administered alongside fibrinolytic therapy.
- Patients also require dual antiplatelet treatment. If there is a high bleeding risk, you can consider aspirin alone or aspirin + clopidogrel. Otherwise, patients are given ticagrelor + aspirin.
- An ECG is done after 60-90 minutes after fibrinolysis has been given – if there is still residual ST elevation, immediate coronary angiography followed by PCI if needed is indicated – this type of PCI is known as rescue PCI (vs primary). The fibrinolysis therapy should not be repeated.
Management – NSTEMI
Patients with an NSTEMI are offered aspirin 300mg alongside fondaparinux, the latter of which should not be given if the patient has a high bleeding risk or if they are going to receive immediate angiography.
- First, the clinical condition of the patient is considered – if they are unstable, they are offered immediate coronary angiography with PCI if indicated. These patients should also be given unfractionated heparin if they are going to undergo PCI.
- If they are stable, a 6-month mortality risk assessment is performed as this will dictate treatment. Those with a risk of >3% can be offered coronary angiography within 72 hours of the first admission. These individuals are treated with dual antiplatelet therapy which is aspirin + prasugrel/ticagrelor if there is no separate indication for oral anticoagulation. If there is a separate indication for oral anticoagulation, they can be given clopidogrel alongside aspirin instead.
Patients with a risk of <3% can be considered for coronary angiography if they are experiencing or demonstrating ischaemia – otherwise they may be managed conservatively with ticagrelor and aspirin, unless they have a high bleeding risk in which case they can be given aspirin alone or aspirin and clopidogrel.
Secondary Prevention of MI
Patients should receive information and education alongside being offered cardiac rehabilitation. Patients should be advised to stop smoking, regularly exercise, stay within the national guidance for alcohol consumption and follow a Mediterranean diet i.e. diet rich in fruit, vegetables and fish. For patients who had hyperglycaemia following an acute coronary syndrome, the risk of developing type 2 diabetes is higher. They should therefore be offered HbA1c testing and be advised of the symptoms of type 2 diabetes, and to consult their GP/PCP if they experience them.
Pharmacological therapy is in the form of:
- ACE inhibitors (or angiotensin receptor blocker if intolerant). Remember to monitor renal function and electrolytes within a week or two of starting this!
- Aspirin + a second antiplatelet agent e.g. clopidogrel/ticagrelor. The second agent is only used for up till 12 months following the MI.
- Beta-blockers to slow the heart down and reduce the myocardial oxygen demand. Diltiazem or verapamil can be considered if beta-blockers are contraindicated.
- Statin – this is at a higher, secondary prevention dose of 80mg
Complications
| Ischaemic | - Failed reperfusion therapy
|
| Arrhythmic | - Ventricular fibrillation
- Ventricular tachycardia
- Atrial fibrillation
- AV node block
|
| Inflammatory | - Pericarditis
- Dressler’s syndrome: Pericarditis following an MI (occurs 1-6 weeks following initial MI)
|
| Mechanic | - Heart Failure
- Cardiogenic Shock
- Left ventricular aneurysm
- Ventricular free wall rupture
- Mitral regurgitation
|
UK Driving Laws Following Myocardial Infarction
For car or motorcycle licence holders, there is no requirement to inform the DVLA of the event. However, patients must be told to stop driving for:
- 1 week with a successful angioplasty
- 4 weeks with an unsuccessful angioplasty
- 4 weeks if did not receive angioplasty
Bus, coach or lorry licence holders do have to inform the DVLA of the MI and also stop driving for 6 weeks.
References
https://www.sciencedirect.com/science/article/pii/B9780124052062000120
https://www.ncbi.nlm.nih.gov/books/NBK459269/
https://academic.oup.com/eurheartj/article/39/2/119/4095042#107689883
https://www.nhs.uk/conditions/coronary-angioplasty/
https://www.nice.org.uk/guidance/CG95/chapter/Recommendations#people-presenting-with-acute-chest-pain
https://www.cvpharmacology.com/thrombolytic/thrombolytic
https://www.nice.org.uk/guidance/cg172/chapter/1-Recommendations#cardiac-rehabilitation-after-an-acute-myocardial-infarction-mi-2
https://www.nice.org.uk/guidance/ng185/chapter/Recommendations
https://emedicine.medscape.com/article/164924-overview
https://patient.info/doctor/dresslers-syndrome
https://www.gov.uk/heart-attacks-and-driving