Cholelithiasis, or gallstones, is the main underlying cause behind biliary colic and cholecystitis.
Cholelithiasis
Cholelithiasis, or gallstones, are stones which develop in the gallbladder. In the vast majority of cases, they cause no symptoms. It is usually when gallstones begin to obstruct parts of the biliary tract do they cause symptoms. They are classified based on their composition:
- Cholesterol: These are mainly comprised of cholesterol and are the most common type of gallstone, accounting for at least 85% of gallstones.
- Pigment: Usually occur secondary to a parasitic or bacterial infection, or due to haemolysis e.g. if a patient has sickle cell anaemia.
- Mixed
Emmanuelm at en.wikipedia, CC BY 3.0 , via Wikimedia Commons
On the right of the image, yellow cholesterol stones can be seen whilst on the left, darker pigmented stones can be seen.
Risk Factors for Gallstones
- Female
- Pregnancy
- Age: 40s
- Obesity
- High Fat Diet
- Prolonged fasting states: Due to risk of overconcentration of bile and thus stone formation
Pathophysiology
- On eating a fatty meal, fat triggers the release of cholecystokinin (CCK) from I cells in the duodenum and jejunum.
- CCK triggers contraction of the gall bladder in order to stimulate release of bile into the duodenum to aid in digestion.
- If there is a gallstone in the gallbladder, contraction can potentially move the stone into the cystic duct (or even the common bile duct).
- As the gallbladder contracts against an impacted stone, the patient experiences pain.
- If this blockage is temporary, it results in biliary colic whilst a more permanent blockage can progress into acute cholecystitis.
Cholesterol Stones
- Cholesterol is held in solution in bile by association with bile salts and phospholipids.
- If the bile becomes highly concentrated with cholesterol, the cholesterol can crystallise and form stones. This is known as cholesterol supersaturation.
- Supersaturation may also occur due to a deficiency of bile salts, meaning there is an inadequacy in agents that can keep the cholesterol soluble.
- This may occur in terminal ileal disease e.g. Crohn’s, as bile salts are reabsorbed at the level of the terminal ileum.
- Abnormal gall bladder motility such that bile remains stagnant e.g. in fasted states is also a potential cause of cholesterol gallstones.
- Oestrogen has been shown to decrease gall bladder motility as well as reduce the synthesis of bile acids, subsequently increasing the amount of insoluble cholesterol in the bile. This may explain the higher risk of gallstones in women, as well as the increased risk seen in women who are pregnant or on oestrogen containing forms of contraception.
Pigement Stones
- Black pigment stones are most often associated with haemolytic anaemias such as hereditary spherocytosis or sickle cell disease as these result in high levels of bilirubin which can form pigment stones.
- Brown pigment stones on the other hand are frequently associated with gallbladder infections.
Clinical Features
When gallstones are symptomatic e.g. whether they are causing biliary colic, cholecystitis or cholangitis, the basic principles of the pain are very similar. Features are usually:
- Right upper quadrant/right hypochondrium pain
- Usually sharp in nature
- Can radiate to the right shoulder (due to irritation of the phrenic nerve), back or epigastrium
- Triggered by fatty meals
- Associated nausea/vomiting
Biliary colic is an acute, painful attack caused by a temporary blockage of the cystic duct by a gallstone. It is a short-lived attack of intermittent pain and may be triggered by eating a heavy meal. Patients can have very painful attacks but are generally physiologically well and lack signs and symptoms of infection.
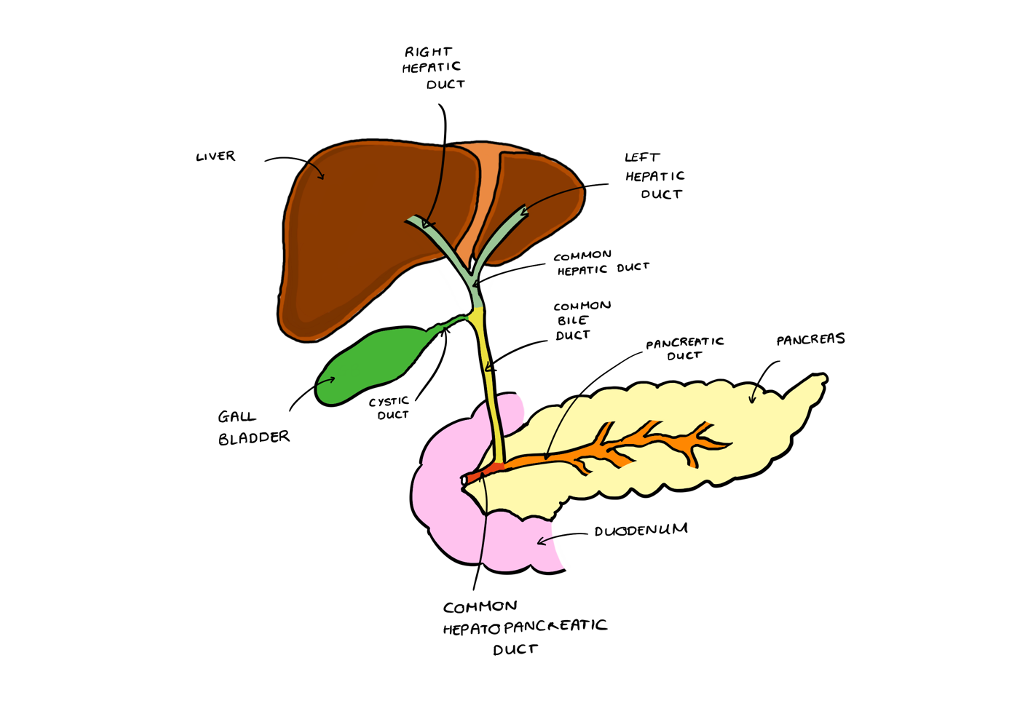
Localising the Blockage
- Having a visual map of the biliary tract in your head is handy to understand where a patient’s symptoms are likely to be coming from.
- Bile is produced by the liver and passes via the hepatic ducts, which meets the cystic duct to form the common bile duct.
- The pancreatic duct from the pancreas then joints the common bile duct later to become the ampulla of Vater, which opens up into the duodenum.
- The control of flow via the ampulla is done through the sphincter of Oddi.
- Jaundice comes from a build up of bilirubin, due to an obstruction in bile flow.
- In the case of biliary colic, there’s no permanent obstruction to bile flow, so jaundice is unlikely.
- In the case of acute cholecystitis, there is an obstruction but not a major one – the common bile duct is still draining so you’re still not as likely to get jaundice.
- In the case of acute cholangitis, you usually have a stone in the common bile duct. This is a major obstruction in bile flow, so you’re much more likely to get jaundice.
Copyright Medic in a Minute 2023
Biliary Tree
Investigations
Bloods
- FBC: May show a raised white cell count in acute cholecystitis.
- LFT: Cholestatic clinical pictures tend to result in a milder increase of the liver transaminases (AST and ALT), but cause greater rises in the ALP and gamma-GT.
- Bilirubin: If raised, suggests cholestasis. If it is above 50, the patient may appear jaundiced.
- Amylase/lipase: An important investigation to rule out acute pancreatitis which also causes abdominal pain radiating to the back, nausea and vomiting. Additionally, gallstones can cause acute pancreatitis.
- INR/Clotting: If bile isn’t moving into the duodenum then it may implicate fat absorption and by consequence, absorption of fat-soluble vitamins e.g. vitamin K which can affect clotting.
- CRP: Marker of inflammation
Imaging
- Abdominal ultrasound
- Abdominal x-ray: Can sometimes show radio-opaque gallstones
- Magnetic resonance cholangiopancreatography (MRCP): This is usually ordered if ultrasound does not detect a stone in the common bile duct, but the bile duct is dilated on abdominal ultrasound and/or there are abnormal liver function tests.
- Endoscopic ultrasound (EUS): This is performed when MRCP does not show anything
Differential Diagnosis
- Biliary colic
- Acute cholecystitis
- Acute cholangitis
- Acute hepatitis
- Acute pancreatitis
- Peptic ulcer disease
- Right lower lobe pneumonia
Management
- Asymptomatic Gallstones: No treatment required
- Symptomatic Gallstones: Laparoscopic cholecystectomy
References
https://www.nice.org.uk/guidance/cg188/chapter/1-Recommendations#diagnosing-gallstone-disease
https://www.ncbi.nlm.nih.gov/books/NBK430772/
https://www.ncbi.nlm.nih.gov/books/NBK459171/
https://www.ncbi.nlm.nih.gov/books/NBK459333/
https://www.ncbi.nlm.nih.gov/books/NBK430834/
https://www.ncbi.nlm.nih.gov/books/NBK459182/