Non-alcoholic fatty liver disease (NAFLD) describes a spectrum of liver disease caused by a build-up of fat in the liver, unrelated to alcohol consumption or other causes of liver disease. This article discusses NAFLD in adults.
Pathophysiology
The underlying pathogenesis of NAFLD is incredibly complex with various factors at play.
- The disease starts off with a combination of environmental and genetic factors that ultimately lead to triglyceride accumulation in the liver. This can be for a range of reasons. For example, insulin normally promotes de novo lipogenesis (making new fats). Thus, insulin resistance = high insulin levels -> lots of new fat production -> fat accumulates in hepatocytes.
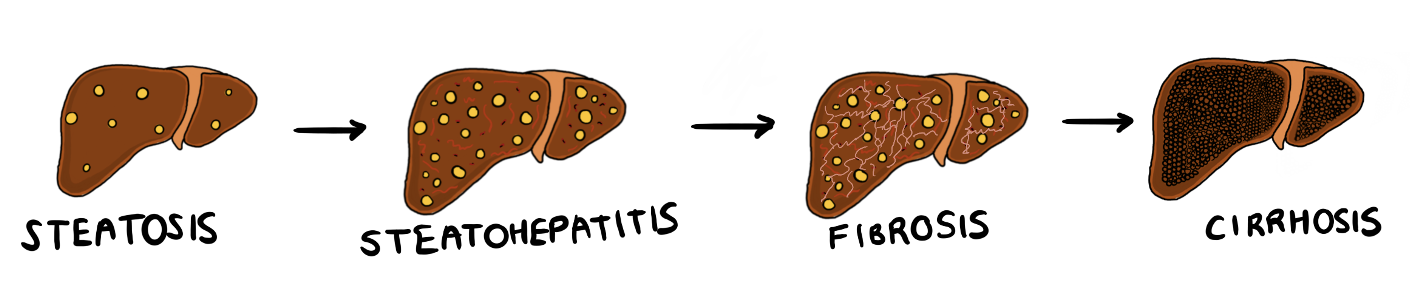
- If the liver accumulates so much fat that at least 5% of the liver contains fat, it’s known as steatosis. On gross examination, the liver appears yellow due to all the large fat droplets accumulating within hepatocytes.
- This fat can also cause inflammation in the liver, and subsequent injury to hepatocytes. At this point, steatosis has now become non-alcoholic steatohepatitis, or NASH. Hepatocytes begin to balloon and swell, and this can be seen on microscopy.
- Over time, all this inflammation caused by lipotoxic substances can lead to apoptosis of hepatocytes which can ultimately progress into fibrosis. If fibrosis continues to advance, patients can develop cirrhosis and end-stage liver failure.
Copyright Medic in a Minute 2022
Schematic Showing Liver Disease Progression
- Normal liver -> Steatosis is rapid but is also reversible.
- Steatosis -> Steatohepatitis and fibrosis takes more time and is less readily reversible.
- Cirrhosis takes years to develop but is usually irreversible.
Risk Factors
- Hypertension
- Type 2 Diabetes Mellitus
- Insulin Resistance
- Obesity
- Hyperlipidaemia
Clinical Features
- Often asymptomatic and is found incidentally
- General symptoms include fatigue or right upper quadrant discomfort
- Hepatomegaly/splenomegaly
- Acanthosis Nigricans
- Signs of Liver Cirrhosis such as:
- Ascites
- Jaundice
- Palmar Erythema
- Spider naevi
- Pruritis
- Dupuytren’s contracture
- Bruising
Investigations
As NAFLD is frequently, it is often an incidental finding, and patients may have normal liver function tests.
Bloods
- Aspartate Aminotransferase (AST) and Alanine Aminotransferase (ALT): Elevated
- AST:ALT Ratio: ALT is usually greater than AST
- Autoantibody screen: Antinuclear antibodies (ANA), Anti-smooth muscle antibodies (SMA), Antimitochondrial antibodies (AMA), Antiobdies to liver kidney microsome type-1 (LKM-1)
- Ceruloplasmin
- Alpha-1 anti-trypsin levels
- Iron studies: Including ferritin and transferrin
- Viral serology: Hepatitis B and C, HIV, EBV, CMV
- Enhanced Liver Fibrosis (ELF) Test: This is a blood test which measures markers of fibrosis. It is offered to patients with confirmed NAFLD to check for advanced liver fibrosis. A score of >= 10.51 + NAFLD is diagnostic of advanced liver fibrosis.
Imaging
- Abdominal/liver ultrasound: In order to visualise steatosis (increased echogenicity).
Special Tests
- Liver biopsy: Highly invasive test but will allow confirmation of steatosis/steatohepatitis.
Management
The ultimate aim is to reduce the disease progression, and if possible, reverse steatosis. Weight loss, diet management, exercise advice, and risk factor management is all important e.g. appropriate management of diabetes, hypertension, hyperlipidaemia etc.
Adults taking statins should continue taking them – however, if liver enzymes double within 3 months of starting a statin, you can consider stopping it.
NICE recommend vitamin E or pioglitazone for adults with advanced liver fibrosis, but this is only considered in a secondary or tertiary care context.
Adults should be monitored every 3 years for advanced liver fibrosis using ELF testing.
References
https://www.ncbi.nlm.nih.gov/books/NBK470243/
https://www.nice.org.uk/guidance/ng49
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5127277/#R37