Hypertension is one of the most common conditions internationally and is a known risk factor for several other co-morbidities such as cardiovascular accidents and cerebrovascular accidents. Essential hypertension describes high blood pressure where the underlying cause is largely idiopathic as opposed to secondary hypertension.
Risk Factors for Essential Hypertension
- Age
- High salt intake
- Obesity
- Sedentary lifestyle
- Excessive alcohol intake
Causes of Secondary Hypertension
Some causes of secondary hypertension include Cushing’s syndrome, primary hyperaldosteronism, pheochromocytoma, aortic coarctation and renal artery stenosis.
Investigations
NICE have produced detailed guidelines on the diagnosis and management of hypertension. Let's start off with the investigations first:
- Clinic blood pressure reading of ≥140/90mmHg, up to 180/120mmHg: NICE guidelines advise a second blood pressure reading be taken if the measurement reads 140/90 mmHg or higher. If the repeat reading is very different, a third reading should be taken and the lowest of the last 2 measurements can be recorded.
- Patients with a confirmed clinic reading ≥140/90mmHg should be offered ambulatory blood pressure monitoring (ABPM) or home blood pressure monitoring (HBPM) if ABPM is not suitable for the patient.
- Patients should also be investigated for target organ damage. This includes conducting a 12-lead ECG, fundoscopy to check for retinopathy, HbA1c, urea and electrolytes, GFR etc.
- A cardiovascular risk assessment using a formal tool should be done e.g. using the QRISK2 tool
- A clinic blood pressure of ≥140/90mmHg and an ABPM/HBPM average of ≥135/85mmHg confirms the diagnosis of hypertension
- Clinic blood pressure reading of ≥180/120mmHg:
- Patients with signs of retinal haemorrhage, papilledema, chest pain, heart failure, acute kidney injury or new onset confusion should be referred for same-day specialist assessment.
- Patients with suspected pheochromocytoma should also be referred for same-day specialist assessment.
- Patients with a blood pressure of 180/120mmHg or higher who have no signs/symptoms that require same-day referral should be investigated for end -organ damage. If there are signs of end organ damage, antihypertensive drug treatment should be started.
- If there are no signs of end organ damage, the blood pressure should be repeated in clinic in 7 days.
Staging Hypertension
NICE have described 3 stages of hypertension, which are defined by a range of blood pressure measurements which are as follows:
- Stage 1:
- Clinic: 140/90mmHg – 159/99mmHg
- ABPM daytime average/HBPM average: 135/85 mmHg – 149/94mmHg
- Stage 2:
- Clinic: 160/100mmHg – 180/120mmHg
- ABPM daytime average/HBPM average: 150/95mmHg or more
- Stage 3:
- Clinic: 180/120mmHg or higher or clinic diastolic blood pressure of 120mmHg or higher
Management
Advising patients with regards to lifestyle is improvement following a diagnosis of hypertension. This should include asking about healthy diet, exercise, alcohol consumption and salt intake.
NICE recommends drug treatment should be offered alongside lifestyle advice when patients have persistent stage 2 hypertension. There are also select groups in which drug treatment can be considered – such as in patients with stage 1 hypertension, under the age of 80 with one of the following: diabetes, target organ damage, renal disease, cardiovascular disease or 10-year cardiovascular disease risk of 10% or more.
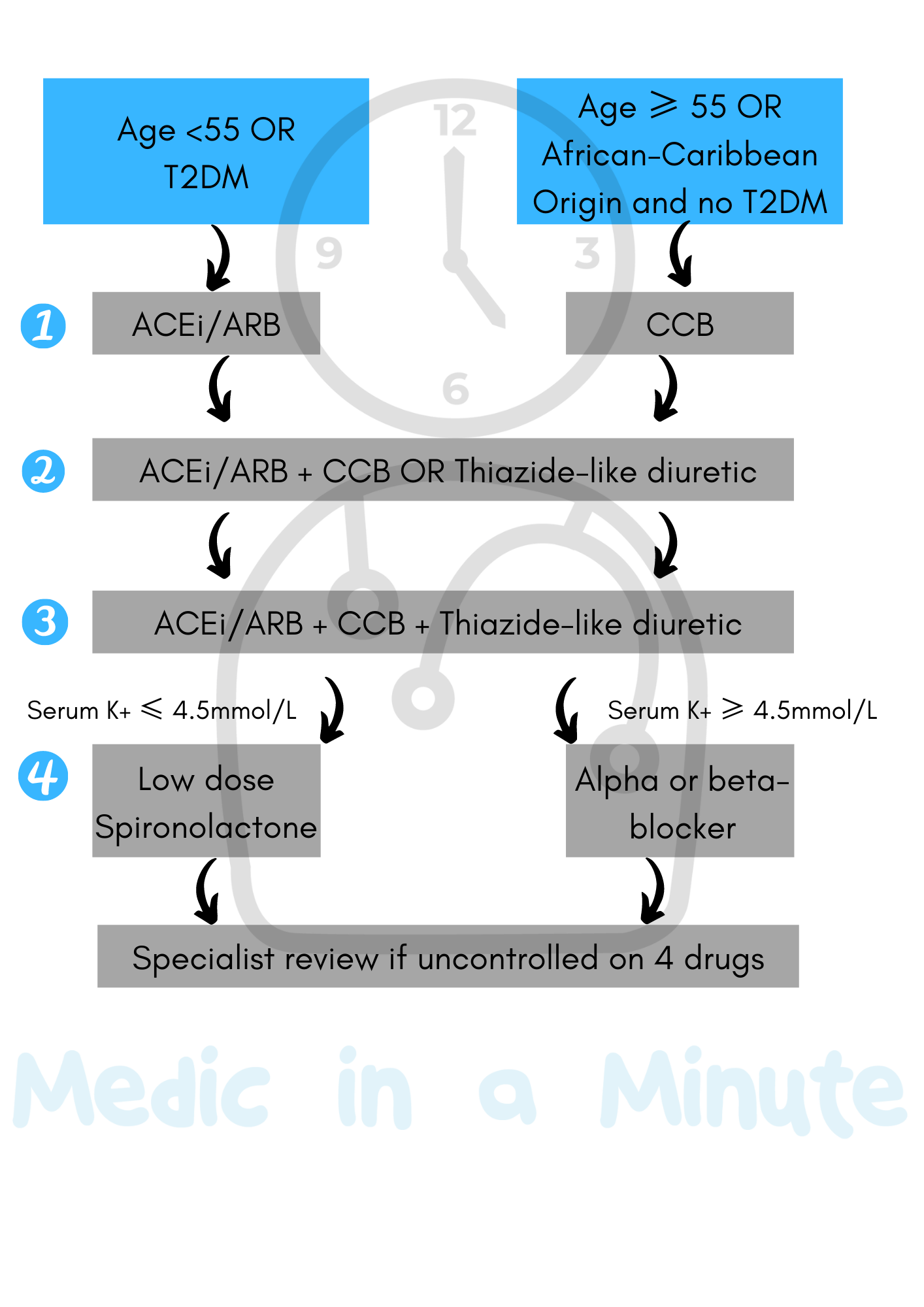
Guidelines lay out hypertension treatment in 4 steps, and largely speaking there are two main patient groups that can be used to understand the guidelines. The following is a very brief and condensed summary of the salient points for hypertension management from NICE NG136.
- Patients with Type 2 Diabetes OR Patients under 55 and not of black African/African-Caribbean origin
- Step 1: Start on ACE inhibitor or ARB. If ACE inhibitor not tolerated, give ARB.
- Step 2: Add a CCB or thiazide-like diuretic if hypertension remains uncontrolled on step 1 treatment.
- Step 3: Offer a combination of ACE inhibitor or ARB, CCB and thiazide-like diuretic
- Step 4: Confirmation that the patient has resistant hypertension is needed e.g. using ABPM again. Patients may benefit from further diuretic therapy, alpha-blockers or specialist advice.
- Patients without Type 2 Diabetes AND over 55 OR Patients without Type 2 Diabetes AND of black African/African-Caribbean origin
- Step 1: Start on CCB. If not tolerated, offer thiazide-like diuretic instead. If patient has evidence of heart failure, start on a thiazide-like diuretic.
- Step 2: Add ACE inhibitor, ARB or thiazide-like diuretic if hypertension remains uncontrolled on step 1 treatment.
- Step 3: Offer a combination of ACE inhibitor or ARB, CCB and thiazide-like diuretic if hypertension uncontrolled on step 2 treatment.
- Step 4: Confirmation that the patient has resistant hypertension is needed e.g. using ABPM again. If the patient definitely has resistant hypertension, a fourth drug could be added, or specialist advice can be sought.
- If serum potassium is ≤4.5mmol/L: Consider adding low dose spironolactone
- If serum potassium is ≥4.5mmol/L: Consider an alpha or beta-blocker
- Specialist review if the hypertension is still uncontrolled on 4 drugs
Copyright Medic in a Minute 2021
Hypertension Management
References
https://www.nice.org.uk/guidance/ng136/chapter/recommendations#identifying-who-to-refer-for-same-day-specialist-review
https://www.ncbi.nlm.nih.gov/books/NBK539859/