This is inflammation of the gall bladder, usually due to an impacted gallstone.
Pathophysiology
- Acute cholecystitis typically occurs when a gallstone becomes lodged and results in blockage – this is usually in the cystic duct or the gallbladder neck.
- In biliary colic, this obstruction occurs but it’s temporary, resulting in a bout of pain followed by relief.
- In acute cholecystitis, the obstruction remains. The gall bladder tissue is secretory so continuous secretions against an obstruction will lead to distension, pain, infection, and inflammation.
- It is possible to develop cholecystitis in the absence of gallstones, known as acalculous cholecystitis. The proposed mechanism for this is if you have gallbladder stasis, bile salts are excessively concentrated in the gallbladder resulting in increased pressure in the organ, ischaemia, bacterial growth, and thus cholecystitis. Causes of this include:
- Extended periods of fasting
- Total parenteral nutrition
- Sepsis
- Extensive trauma
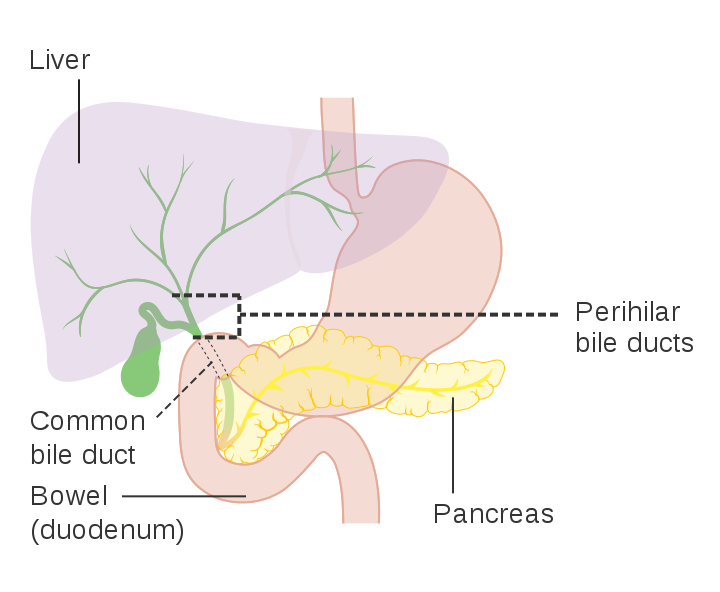
Cancer Research UK, Public domain, via Wikimedia Commons
Biliary Tract
Clinical Features
- Abdominal Pain: Starts similar to biliary colic i.e. right upper quadrant pain. Difference being, it will be continuous rather than colicky in nature.
- Right shoulder tip pain: Due to irritation of the diaphragm
- Nausea/vomiting
- Fever
- Right upper quadrant mass: Not always felt
- Murphy’s sign positive: Place hand over the right upper quadrant and asking the patient to take a deep breath. As the inflamed gall bladder makes contact with the examiner’s hand, there will be sudden pain and the patient will have an abrupt arrest in inspiration.
Investigations
Bloods
- FBC: Looking for raised white cells
- LFT: ALP, gamma-GT elevation (an obstructive picture). Bilirubin may also rise.
- CRP: Raised
- U&Es, Bone Profile: Baseline
- Amylase: Rule out acute pancreatitis
- VBG: As part of work-up for an acute abdomen or if there’s suggestion of sepsis with a gall bladder source
Imaging
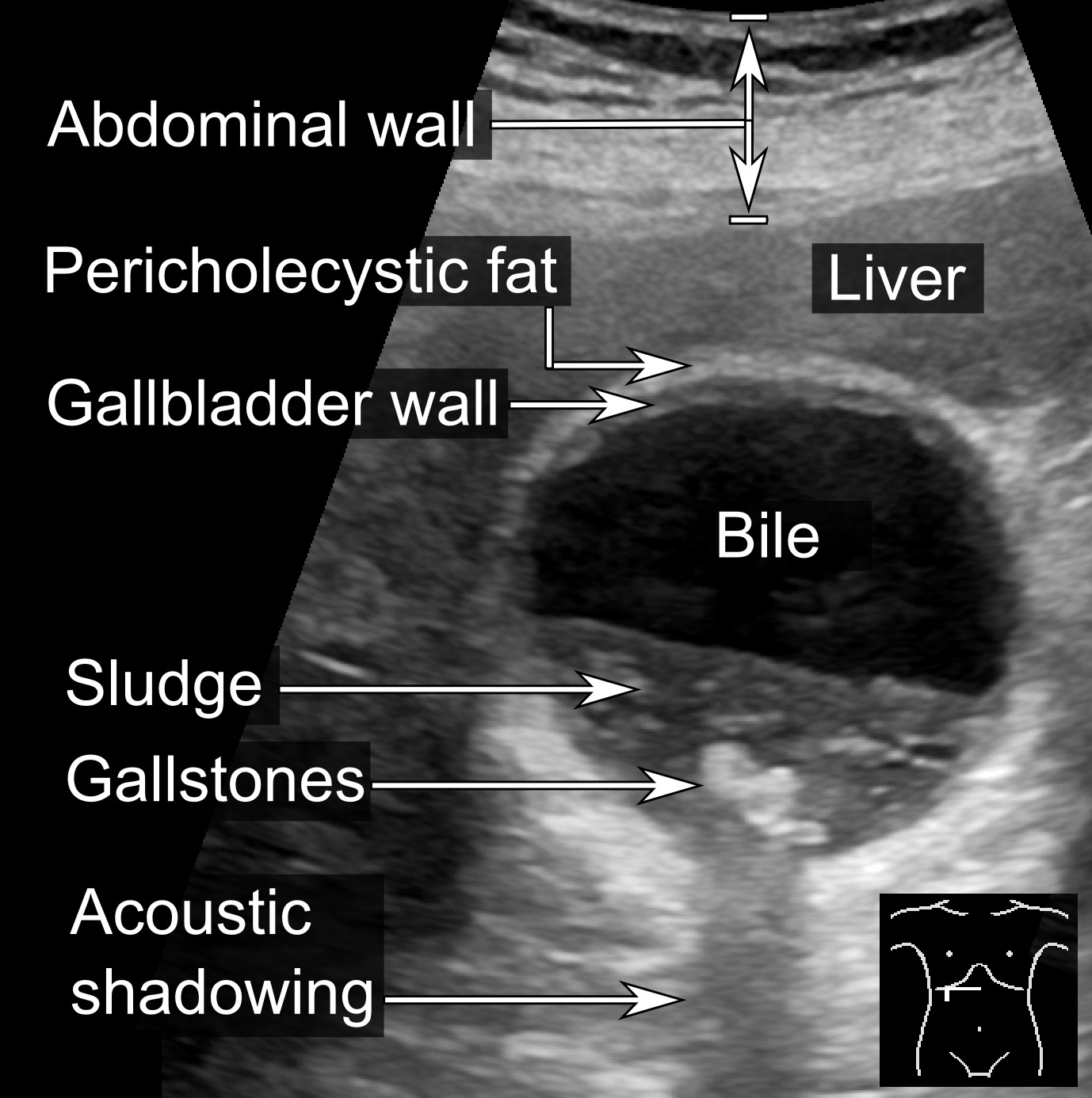
- Abdominal ultrasound: Looking for gallstones and thickening of the gall bladder wall.
- Magnetic resonance cholangiopancreatography (MRCP): Provides a more detailed image of the biliary tree – used when a stone in the common bile duct is being suspected.
- CT Abdomen and Pelvis with contrast: If suspecting gall bladder perforation
Mikael Häggström, M.D. Author info - Reusing images- Conflicts of interest: NoneMikael Häggström, M.D.Consent note: Written informed consent was obtained from the individual, including online publication., CC0, via Wikimedia Commons
Ultrasound Imaging of Gallstones and Biliary Sludge
Management
Management in an inpatient setting is usually conservative unless patients are severely unwell/septic.
Supportive
- IV Fluids
- Analgesia
- Antibiotics (Oral or IV depending on severity)
Surgical
Patients with acute cholecystitis will eventually require laparoscopic cholecystectomy as they’re likely to have recurrent episodes. NICE recommend that this be within 1 week of diagnosis. Some centres may choose to do this whilst the patient is admitted, whilst others will delay the surgery to happen as an outpatient procedure, to allow the acute episode to settled.
Patients who develop intra-abdominal collections secondary to cholecystitis may require drainage.
Complications
- Empyema: Occurs when the gallbladder becomes filled with pus. This can progress into gangrene of the gallbladder and potentially even rupture which can cause the patient to become septic.
- Gallbladder Rupture
- Gallbladder Gangrene
- Cholecystocutaneous fistula: A fistula between the gallbladder and the skin.
- Gallstone ileus: A rare type of small bowel obstruction whereby a fistula forms between an inflamed gallbladder and the adjacent intestinal structures, enabling passage of a gallstone into usually the duodenum.
References
https://link.springer.com/content/pdf/10.1007%2Fs00534-012-0564-0.pdf
https://www.ncbi.nlm.nih.gov/books/NBK459171/
https://www.nice.org.uk/guidance/cg188/chapter/1-Recommendations#diagnosing-gallstone-disease
https://www.augis.org/wp-content/uploads/2014/05/Acute-Gallstones-Pathway-Final-Sept-2015.pdf