Chronic obstructive pulmonary disease (COPD) is a disorder affecting the lungs. Airways become obstructed, and there is little to no reversibility of this obstruction.
Risk Factors
- Smoking, including second-hand smoke
- Air pollution
- Occupational irritants e.g. silicia dust, flour dust, welding fumes and coal dust
Chronic Bronchitis and Emphysema
Two main conditions fall under the umbrella of COPD – chronic bronchitis and emphysema.
Chronic bronchitis is where patients produce excessive amounts of mucus in response to certain toxins. Patients with chronic bronchitis are prone to infections due to the risk of this stagnant mucus become infected. Emphysema is a lung condition where there is a structural disruption of the lung tissue.
Chronic Bronchitis Pathophysiology
- An initial noxious stimulus such as cigarette smoke, bacterial infection, viral infection or another toxin, causes inflammation in the lungs.
- This promotes hypertrophy and hyperplasia of mucous glands in the bronchi. The numbers of goblet cells in the respiratory epithelium also increase, resulting in mucus hypersecretion.
- Smoking also makes cilia on the epithelium shorter and reduces their motility.
- The consequence of this excessive mucus and inability to clear it leads to airway obstruction.
- Patients also become prone to infections due to stagnant mucus that can’t be cleared.
- Chronic irritation of the airway leads to thickening of the bronchial wall, increasing airway obstruction.
- Airway obstruction has two major consequences. Firstly, it is difficult getting oxygen into the airways due to these large mucus plugs, leading to hypoxia. It is also difficult to get carbon dioxide out of the airways, resulting in carbon dioxide retention, or hypercapnia. Patients produce extra red blood cells in order to compensate for the hypoxia, which can cause a polycythaemia.
- Due to the increased bulk of mucus glands, the Reid index can be measured to diagnose chronic bronchitis. This is the ratio of the thickness of bronchial mucus glands relative to the total airway thickness, from the epithelium to the cartilage. Normally, this should be <0.4, but is increased in chronic bronchitis.
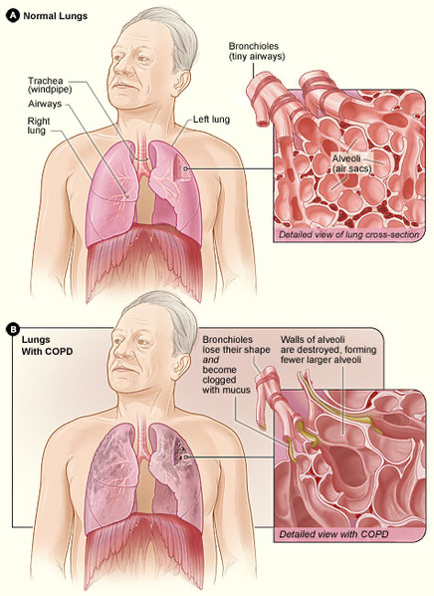
National Heart Lung and Blood Institute, Public domain, via Wikimedia Commons
COPD Pathophysiology
Emphysema – Pathophysiology
- Noxious stimuli such as cigarette smoke activate macrophages, which recruit neutrophils and other inflammatory cells to the lungs.
- Macrophages and neutrophils cause the release of tissue proteases such as elastases and matrix metalloproteinases which damage the elastic fibres found within alveoli.
- Elastin fibres which normally allow expansion and recoil of the alveoli are damaged, resulting in collapse of alveoli which can no longer hold themselves open during exhalation due to loss of recoil.
- This results in air trapping in the alveoli, as air cannot be fully expelled resulting in increased total lung capacity. Air trapping significantly increases the work of breathing for patients.
- Septa between alveoli break down, leading to the coalescing of alveoli and reduced surface area for gas exchange. If these become sufficiently large, they can form large emphysematous blebs or bullae. These are problematic as if they rupture, they will cause a pneumothorax.
Emphysema can also be caused by alpha-1 antitrypsin deficiency, a deficiency in an enzyme which inhibits elastases in the lungs. Deficiency in this anti-protease enzyme will therefore lead to breakdown of lung tissue.
There are three main patterns of emphysema:
- Centriacinar: Associated with smoking. Affects the respiratory bronchioles and the central part of the acinus, sparing the distal aspect of the alveoli. Mainly found in upper lobes.
- Panacinar: Associated with alpha-1 antitrypsin deficiency where the entire acinus is affected, and mainly affects the lower lobes.
- Paraseptal or Distal Acinar: Distal aspect of the acinus such as alveolar duct and alveoli are affected. Tends to occur in the peripheral aspects of the lung near the pleura. This type is thought to be the main culprit behind spontaneous pneumothorax.
Clinical Features
| Chronic Bronchitis | Emphysema |
| Productive cough present for most days for 3 months of 2 consecutive years | May have a cough but less sputum production |
| Expiratory wheeze due to bronchoconstriction and mucus plugs | Air trapping resulting in barrel chest and pursed lip breathing |
| Polycythaemia | Hyper resonant percussion notes |
| Coarse crackles on auscultation due to air flowing through mucus filled airways | Dyspnoea, tachypnoea |
| Dyspnoea, tachypnoea | Weight loss and cachexia |
- Pulmonary hypertension can develop due to COPD and is more commonly seen in chronic bronchitis.
- In areas of reduced alveolar ventilation, for example amongst alveoli that are distal to a mucus plug, reflex vasoconstriction of blood vessels occurs – this is normal respiratory physiology.
- If this begins to happen on a widespread scale across the lungs, vascular resistance due to significant vasoconstriction occurs, leading to pulmonary hypertension.
- Over time, this will increase the work for the right side of the heart which needs to pump against a higher resistance, leading to right sided heart failure secondary to a lung condition. This is known as cor pulmonale.
MRC Dyspnoea Scale
| Grade | Description |
| 1 | Not troubled by breathlessness except on strenuous exercise |
| 2 | Short of breath when hurrying on the level or walking up a slight hill |
| 3 | Walks slower than most people on the level, stops after a mile or so, or stops after 15 minutes walking at own pace |
| 4 | Stops for breath after walking about 100 yds or after a few minutes on level ground |
| 5 | Too breathless to leave the house, or breathless when undressing |
Investigations
Bedside
- ECG: Looking for signs of right sided heart failure
- Sputum Culture: If considering an infective exacerbation of COPD
Bloods
- Full blood count: Polycythaemia
- ABG: Looking for hypoxia/hypercapnia
Imaging
- Chest x-ray: Exclude other diseases and also look for signs of COPD such as hyperinflation which can be seen by flat hemidiaphragms.
Special Tests
- Spirometry
- FEV1/FVC < 0.7 to indicate an obstructive pattern
- Reduced FEV1
- Can measure post-bronchodilator reversibility in order to rule out asthma (as in asthmatics, the airway obstruction is reversible)
Management
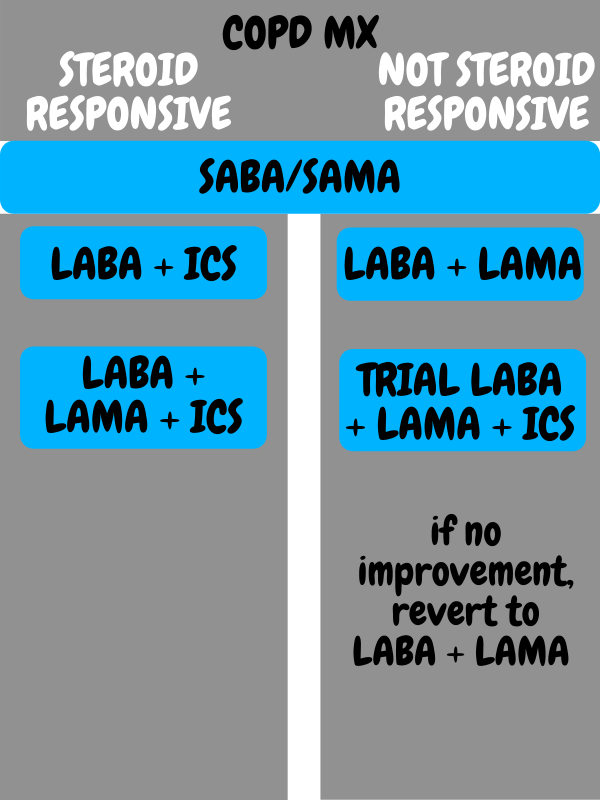
All patients should be offered smoking cessation advice and pneumococcal and influenza vaccinations. If appropriate, pulmonary rehabilitation can be offered.
- Short-acting beta-2 agonist (SABA) e.g. salbutamol
- Short-acting muscarinic antagonist (SAMA) e.g. ipratropium bromide
- Long-acting beta-2 agonist (LABA) e.g. salmeterol
- Long-acting muscarinic antagonist (LAMA) e.g. tiotropium bromide
- Inhaled corticosteroid (ICS) e.g. fluticasone, budesonide, beclomethasone
Based on UK NICE guidelines, patients are offered a short-acting bronchodilator as the first step in inhaled therapy. This can be either a SABA or SAMA.
If patients are still symptomatic or having exacerbations despite being on a short-acting bronchodilator alongside non-pharmacological treatment such as smoking cessation and vaccines, additional treatment is given based on if the patient has asthmatic features to their COPD such as:
- Diurnal variation of at least 20% in peak expiratory flow
- At least 400ml variation in FEV1 over time
- History of atopic disease
- High eosinophil count
as these would suggest steroid responsiveness.
Asthmatic Features
- LABA + ICS
- If the patient is still having symptoms which affect quality of life, or they have had 1 severe exacerbation or 2 moderate exacerbations in a year, LABA + ICS + LAMA is offered.
No Asthmatic Features
- LABA + LAMA
- If the patient is still having symptoms which affect quality of life, you can consider a 3-month trial of LABA + LAMA + ICS, but revert back to LABA + LAMA if there’s no improvement after this trial period.
- If the patient has had either 1 severe, or 2 moderate exacerbations in a year, LABA + LAMA + ICS can be considered.
Other Treatments
- Mucolytics e.g. carbocisteine, dornase alfa or bromhexine.
- Prophylactic antibiotics may be needed if patients are having recurrent exacerbations
- Physiotherapy
Copyright Medic in a Minute 2021
COPD Management Quick Reference Guide
Long-Term Oxygen Therapy
LTOT must be given with extreme care in patients with COPD, as these individuals typically rely on their hypoxic drive to breathe. Thus, inappropriate prescription could lead to respiratory depression.
Severe symptoms may warrant consideration for LTOT such as cor pulmonale or oxygen saturations of <92% on air. Patients are assessed for LTOT through the measuring of ABG on 2 separate occasions at least 3 weeks apart. As per NICE guidance, who do not smoke and have a PaO2<7.3kPa when stable, or patients with PaO2 7.3-8kPa + either polycythaemia, peripheral oedema or pulmonary hypertension are considered for LTOT.
References
https://www.nice.org.uk/guidance/ng115/chapter/Recommendations#diagnosing-copd
https://thorax-bmj-com.iclibezp1.cc.ic.ac.uk/content/thoraxjnl/74/1/4.full.pdf
https://www.atsjournals.org/doi/full/10.1164/rccm.201210-1843CI
https://www.ncbi.nlm.nih.gov/books/NBK482437/
https://www.atsjournals.org/doi/pdf/10.1513/pats.200708-126ET
https://emedicine.medscape.com/article/297664-overview#a3
https://mrc.ukri.org/research/facilities-and-resources-for-researchers/mrc-scales/mrc-dyspnoea-scale-mrc-breathlessness-scale/
Fletcher CM. The clinical diagnosis of pulmonary emphy- sema—an experimental study. Proc R Soc Med 1952;45: 577–584.