Primary sclerosing cholangitis (PSC) is a type of liver disease which affects biliary ducts. It tends to present in 30s-40s, and affects men more commonly than women.
Pathophysiology
The precise pathophysiology of PSC is still unknown, but a multifactorial process is currently theorised as the underlying cause, with a combination of genetics, the environment and the immune system likely playing a role in the development of PSC.
The basic understanding at present is genetically predisposed individuals have a response to an unknown environmental trigger, which leads to injury to the cholangiocytes that line intra-hepatic and extra-hepatic bile ducts. Subsequent inflammation and scarring (fibrosis) occur within these ducts which causes them stricture. It’s also possible for ducts to fibrose so much that they are completely obliterated. Thus, patients with PSC get reduced bile flow, or cholestasis.
There is a major link between inflammatory bowel disease and PSC, particularly ulcerative colitis – this is thought to be as high as 70%.
Clinical Features
- Usually asymptomatic in its early stages, and patients are only diagnosed incidentally due to abnormal liver function tests.
- Fatigue
- Intermittent jaundice
- Pruritis
- Right upper quadrant pain
- Weight loss
- Hepatomegaly or splenomegaly
- Signs and symptoms of inflammatory bowel disease
Investigations
Bloods
- Liver function tests: Alkaline phosphatase (ALP) is mainly elevated in PSC, with gGT, ALT and AST also elevated.
- Autoantibody Tests: Many patients test positive for the following antibodies
- Antinuclear antibodies (ANA)
- Anti-smooth muscle antibodies (ASMA)
Imaging
- Magnetic resonance cholangiopancreatography (MRCP): This is the imaging modality of choice for investigating PSC.
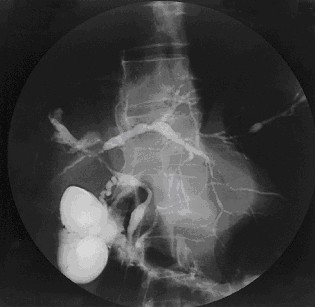
- Classic ‘beads-on-a-string’ appearance with the string being areas of narrowing/strictures and the beads being the normal or slightly dilated duct.
- This is seen for intra-hepatic and extra-hepatic ducts.
Joy Worthington, Roger Chapman, CC BY 2.0 , via Wikimedia Commons
Cholangiogram of PSC
Special Tests
- Liver biopsy: This is not used as much in practice, though it’s useful for diagnosing small duct PSC as picking up PSC in the smaller ducts is more difficult with regular imaging. The classic finding is an ‘onion skin’ fibrosis, due to the fact the fibrosis that occurs in PSC happens in concentric layers.
Management
There is no particular management for PSC at present, and current treatment revolves around symptom management. For example, large strictures can be dilated via ERCP in order to reduce symptoms of cholestasis such as pruritis. End-stage disease may be managed through liver transplantation.
Complications
Monitoring patients for cancer is also extremely important, as patients with PSC are at higher risk of bile duct, hepatic, colonic and gallbladder cancers. Patients may also develop bacterial cholangitis, portal hypertension and ascites.
References
Chapman R, Cullen S. Etiopathogenesis of primary sclerosing cholangitis. World J Gastroenterol. 2008 Jun 7;14(21):3350-9.
https://www.bsg.org.uk/wp-content/uploads/2019/11/Diagnosis-and-Management-of-PSC_gutjnl-2018-317993.pdf?x25809
https://journals.lww.com/ajg/Fulltext/2015/05000/ACG_Clinical_Guideline__Primary_Sclerosing.10.aspx
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6394256/
https://www.pscsupport.org.uk/complications-in-psc/