Herpes zoster, also known as shingles, is a viral infection which occurs following reactivation of a dormant varicella zoster virus.
Pathophysiology
- Varicella zoster is a type of herpes virus which is more commonly known to cause chickenpox.
- Say someone gets chickenpox in their early life (due to varicella zoster). The varicella zoster virus is able to remain dormant within dorsal root ganglia of spinal nerves or sensory ganglia of cranial nerves.
- At any point, the virus can become reactivated e.g. through immunosupression.
- If varicella zoster does become reactivated, it results in shingles.
- It is also possible to catch the shingles virus through direct skin contact or inhalation of infectious droplets,
- If someone has not been exposed to varicella zoster previously and catches the varicella zoster virus from someone who has shingles, it'll simply cause chickenpox.
- Once lesions crust over, it’s thought that they’re no longer infectious
Clinical Features
- Prodrome: Patients may experience this prior to developing a rash. Symptoms include:
- Fever
- Malaise
- Headache
- Pain in affected dermatome (burning/throbbing): As the infection usually affects a dorsal root ganglion, the symptoms tend to appear in a dermatomal pattern.
- Rash
- Itchy
- Maculopapular rash which develops into vesicles
- Erythematous
- Arise in crops along a dermatome
- Do not cross the midline
- Thoracic and cervical dermatomes are most commonly affected
- Zoster sine herpete: Pain of shingles but no rash
- Paraesthesia
M.S., Public domain, via Wikimedia Commons
Shingles Rash
Herpes Zoster Ophthalmicus
- This describes varicella zoster reactivation in the trigeminal nerve.
- It is important to look out for Hutchinson’s sign which is a rash on the tip of the nose as this suggests infection of the ophthalmic branch of the trigeminal nerve and impending inflammation of the eye.
- This is a concern as it can be sight-threatening.
- Patients with visual symptoms e.g. photophobia/eye pain/red eye, or suggested involvement of the ophthalmic branch should be referred to a specialist or hospital as complications may be severe such as corneal ulceration and sight loss.
Investigations
The diagnosis is largely clinical although a PCR can be performed on the lesions. A blood PCR may be particularly useful in cases of zoster sine herpete.
If shingles occurs in someone who is otherwise healthy, it should prompt investigation for underlying immunocompromise e.g. HIV/malignancy.
Management
If patients have a serious infection e.g. an immunocompromised individual with a widely disseminated rash or someone with eye involvement, a hospital admission may be warranted.
Alternatively, oral antivirals such as aciclovir, famciclovir or valaciclovir can be prescribed, ideally within 72 hours (this can be extended in some instances) of the rash appearing, alongside analgesics.
A range of analgesics can be used. NICE recommend the following:
- Start with paracetamol alone or paracetamol + codeine/NSAID
- If this doesn’t work, drugs for neuropathic pain such as gabapentin or pregabalin can be used.
- Oral corticosteroids may also be used alongside an antiviral in immunocompetent patients
General advice also includes:
- Avoid contact with people who haven’t had chickenpox before
- Avoid sharing towels and clothes
- Avoid contact with pregnant women, immunocompromised people, and babies < 1 month
Complications
- Post Herpetic Neuralgia: residual chronic and recurrent pain, paraesthesia and abnormal sensation in the affected region after the rash has healed.
- Scarring: Hypo/hyperpigmentation in the areas affected by the rash
- Herpes Zoster Encephalitis: This is a potential complication of a herpes zoster infection, presenting with features of a herpes zoster infection in addition to features of encephalitis i.e. altered mental status.
- Vision loss: If ophthalmic shingles is not treated
- Ramsay Hunt Syndrome
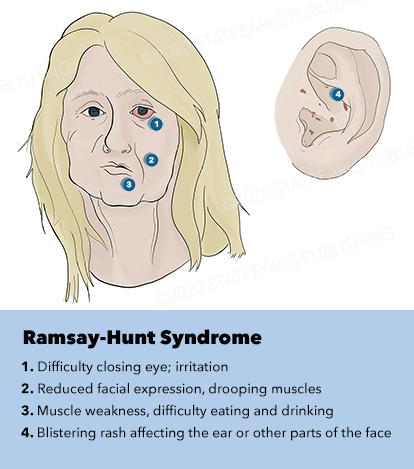
Ramsay Hunt Syndrome
Ramsay Hunt is a complication of a shingles infection, and occurs when the geniculate ganglion of the facial nerve is affected by the virus, resulting in the following signs and symptoms which occur on the affected side (ipsilaterally):
- External auditory canal rash +/- on the hard palate/anterior two thirds of the tongue
- Facial palsy: May be recognised by the loss of the nasolabial fold/drooping of the eyebrow/drooping of the corner of the mouth
- Loss of taste: Facial nerve supplies the anterior two thirds of the tongue
- Vertigo
- Tinnitus
- Drooling
- Hyperacusis: The facial nerve supplies the stapedius muscle which is involved in the stapedius reflex, which results in contraction of the stapedius in response to an intense sound stimulus.
- Dry-eye: Inability to close the eye can result in a dry eye, so artificial tears may be required
It requires treatment with oral antivirals – oral steroids can sometimes be used alongside antiviral therapy.
Ella Workman, CC BY 4.0 , via Wikimedia Commons
Features of Ramsay Hunt Syndrome
References
https://www.facialpalsy.org.uk/causesanddiagnoses/ramsay-hunt-syndrome/
https://cks.nice.org.uk/topics/shingles/management/management/
https://academic.oup.com/ageing/article/46/5/872/3868053
Davidson's Principles and Practice of Medicine Twenty-Third Edition – Infectious disease chapter 11
https://www.mayoclinic.org/diseases-conditions/shingles/symptoms-causes/syc-20353054
https://open.umich.edu/sites/default/files/downloads/acoustic__stapedius__reflexes.pdf