Dementia is a typically chronic and progressive neurodegenerative condition affecting various higher functions including memory, concentration and behaviour. Alzheimer’s disease (AD) is the most common cause of dementia.
Types of Dementia
- Alzheimer’s
- Lewy Body
- Fronto-temporal
- Vascular
Progressive Process
The onset of dementia is gradual, and can be thought of as having 3 major stages – pre-clinical, prodromal/mild cognitive impairment, and dementia.
- Pre-Clinical: This is where you start to see subtle changes e.g. episodic memory losses (recalling personal memories), slight changes in behaviour such as apathy/mild irritability, and reduced learning curves.
- Mild Cognitive Impairment: This is where a dysfunction is more apparent and may start to concern the patient or their family. There is more obvious interruption to memory, learning, recall, and behaviour.
- Dementia: Dementia is the point at which cognitive impairments begin to interfere with activities of daily living.
Pathophysiology
The precise underlying aetiology of Alzheimer’s is not yet known, though it is likely to be multifactorial in nature. The current understanding of the pathophysiology is based around two main things:
- Extracellular beta-amyloid plaques: These are produced by the processing of the amyloid precursor protein (APP). Mutations in the gene that encodes for the APP protein have been linked to the development of Alzheimer’s.
- Intracellular neurofibrillary tangles: These are intracellular collections which are thought to arise due to increased phosphorylation of the tau protein.
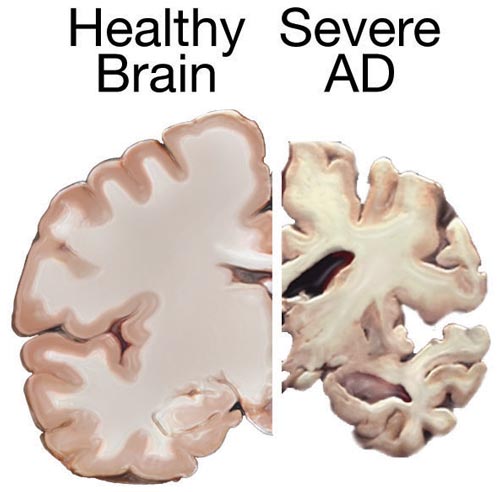
- These plaques and tangles together are thought to result in neuronal cell death and atrophy of the brain, which thus manifests in various cognitive and non-cognitive symptoms. This can sometimes be seen on imaging, particularly atrophy of the temporal lobes.
- This degeneration tends to start in the hippocampus, which is mainly involved in memory as well as learning, which is why AD tends to start with subtle memory and learning difficulties.
National Institutes of Health, Public domain, via Wikimedia Commons
Brain Atrophy in Alzheimer's
Risk Factors
- Increasing age: Symptoms tend to start >65
- Family history
- History of traumatic head injury, particularly repetitive head injury e.g. from boxing
- Genetic risk factors
- Trisomy 21
- Huntington’s disease
- Mutations in APP gene found on chromosome 21
- Mutations in Apolipoprotein E (APOE) gene found on chromosome 19: This gene encodes the apolipoprotein E protein. It is though that fragments of this protein affect mitochondrial functioning resulting in a toxic effect to the brain. The APOE4 allele in particular is linked to Alzheimer’s disease whilst the APOE2 allele has been found to be protective.
- Mutations in presenilin I (PSEN1) gene found on chromosome 14
- Mutations in presenilin II (PSEN2) gene found on chromosome 1
- Cerebrovascular disease
- Vascular risk factors: Hyperlipidaemia, obesity, smoking, stroke, hypertension, history of stroke or MI
Protective Factors
- Exercise
- Higher educational level
- Higher levels of professional achievement
- Mediterranean diet
Clinical Features
Alzheimer’s is a progressive condition, so symptoms tend to start off mild and get worse with time.
- Memory loss:
- Usually begins as short-term memory problems e.g., asking the same question multiple times, forgetting appointments/names/places
- Also tends to affect episodic memory
- Disorientation to time, place and person e.g., patients may find they get lost in places
- Misplacing items
- Difficulty with complex tasks, judgement and decision making e.g., trouble handing finances
- Problems with higher cognitive function: Known as the 5 A symptoms
- Apraxia: Difficulty carrying out purposeful/coordinated tasks e.g., dressing or brushing hair
- Agnosia: Inability to recognise familiar objects or faces
- Aphasia/Dysphasia: Difficulty to express speech
- Anomia: Inability to remember the names of items/things
- Amnesia: Memory disturbance
- Behavioural and psychiatric changes of dementia (BPSD):
- Behavioural:
- Irritability/agitation
- Apathy
- Disinhibition
- Motor disturbances: Restlessness/pacing
- Sleep disturbances
- Repetition
- Psychiatric
- Mood disorders: Depression
- Psychosis: Hallucinations or delusions
Differential Diagnosis
- Delirium: An acute impairment in cognition caused by an underlying problem e.g. dehydration, infection etc
- New hearing/visual impairment
- Depression
- Hypothyroidism/Hyperthyroidism
- Drugs: Certain drugs such as benzodiazepines and opiates can result in cognitive changes
- Normal pressure hydrocephalus: Can result in cognitive impairment
- B12 deficiency
Investigations
Bedside
- History and Examination: Remember, if you cannot take a history from the patient, get a collateral!
- Urine Dip: UTI as an acute cause of cognitive dysfunction (delirium)
Bloods
- FBC, U&E, LFTs: Baseline
- Calcium: Hypercalcaemia can cause neuropsychiatric changes
- TFTs: Thyroid dysfunction as a possible cause of confusion
- Folate and B12 levels
Imaging
- CT/MRI: Rule out structural causes of confusion
Cognitive Assessment
- MoCA Test: Used to assess for mild cognitive impairment. Looks at memory, visuospatial tasks, language, orientation, and a few other things.
- 10-CS: 10-point cognitive screener
- Asks about orientation (date, month, year), word recall, and an animal naming task
- 6CIT: 6-item cognitive impairment test
- Looks at recall, counting, and months of the year
Specialist Diagnostic Services Assessment
As per NICE CKS, patients should be referred to a specialist dementia diagnostic service e.g. a memory clinic if reversible causes of cognitive decline have been excluded and there is still a suspicion of dementia
Management
Conservative
- Manage modifiable risk factors e.g. hypertension, obesity, smoking etc
- Cognitive stimulation therapy: Typically group-based therapy where different activities are done e.g. doing puzzles/games/playing instruments
- Packages of care: Considering the need for carers – OD, BD, TDS, QDS, live-in carer, or considering placement in a nursing home
- Future Planning
- Advance care plans: Considering where a patient may wish to be should they become unwell, who would look after them etc
- Lasting power of attorney (LPA): There are two types of this – health, and finances. An LPA acts as an advocate for a patient who no longer has capacity – they make decisions based on what that individual would have wanted if they had capacity
- Resuscitation: Discussions surrounding resuscitation status
Medical
These mechanisms of actions are super simplified, but if you’re interested you can read more in the references.
- Acetylcholinesterase (AChE) inhibitors:
- MOA: Work to increase levels of Ach. Current theories suggest increased cholinergic activity in the hippocampus is associated with improved memory and learning processes. It’s also thought to have an anti-inflammatory effect that may be present secondary to excessive beta-amyloid.
- They aren’t usually used in severe disease
- Examples: Donepezil, Galantamine, Rivastigmine
- Memantine:
- MOA: NMDA receptor activation by glutamate in the CNS is thought to strengthen synapses. There is a theory of glutamate excitotoxicity whereby excessive glutamate results in various negative outcomes such as excess free radicals and promotion of apoptosis. Memantine is an antagonist of glutamatergic NMDA receptors.
- Usually used when patients cannot be given AChE inhibitors or in more severe disease
Driving
For patients with dementia, group 1 (cars and motorbikes) licence holders need to inform the DVLA who then decide if someone can continue driving. A group 2 (lorries and buses) licence holder cannot drive and needs to inform the DVLA.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2685260/
https://practicalneurology.com/articles/2019-june/preclinical-prodromal-and-dementia-stages-ofalzheimers-disease
https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-019-0524-y#Sec12
https://cks.nice.org.uk/topics/dementia/management/suspected-dementia/
https://www.oaepublish.com/neurosciences/articles/2347-8659.167305/