The thyroid gland is a butterfly shaped gland found anterior to the trachea in the neck. It produces thyroid hormone which has a widespread role in the body affecting multiple bodily functions including metabolism and growth.
Three main hormones are produced by the thyroid:
The vast majority of T3 and T4 hormone is bound to transport proteins in the serum, including thyroxine-binding globulin (TBG) and albumin. It is the amount of free (unbound) T3 hormone which is truly active.
Thyroid hormone homeostasis begins at the hypothalamus. The axis works in the following way:
1. The periventricular nucleus (PVN) of the hypothalamus releases thyroid releasing hormone (TRH) into the hypothalamo-hypophyseal portal system to get to the anterior pituitary gland.
2. TRH stimulates release of thyroid stimulating hormone (TSH) from the anterior pituitary gland.
3. TSH binds to receptors on follicular cells of the thyroid gland, resulting in increased levels of serum T3 and T4.
4. T3 and T4 work to increase metabolic and cellular activity. Some actions of their actions include:
5. TRH also stimulates prolactin production from the anterior pituitary which can cause lactation and growth of breast tissues.
Thyroid Hormonal Axis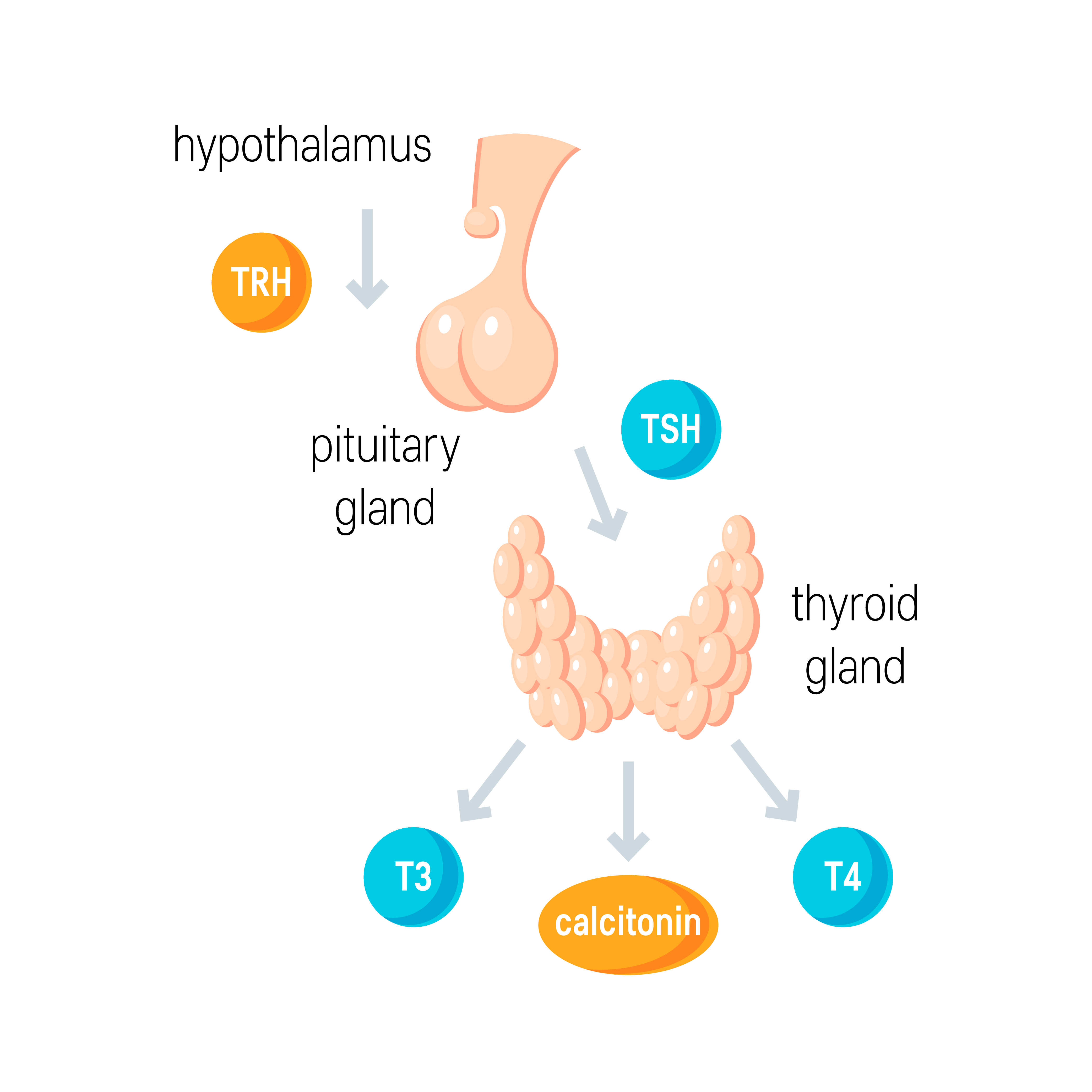
Various causes exist for hypothyroidism. These include:
Primary Causes: The thyroid gland itself is dysfunctional
Secondary/Tertiary Causes: The pituitary or hypothalamus is dysfunctional (respectively):
You can think of the signs and symptoms of hypothyroidism indicating a ‘slowing down’ of bodily functions e.g.
Other features include:
Menstruation can be a bit confusing with hypothyroidism. Although we commonly consider hypothyroidism as a ‘slowing down’ of functions, with menstruation, women tend to experience menorrhagia in hypothyroidism vs amenorrhoea in hyperthyroidism.
Bedside
Bloods
| TSH | T3/T4 | Interpretation |
| High | Low | Primary Hypothyroidism |
| High | Normal | Subclinical Hypothyroidism |
| Low | Low | Central (Secondary/Tertiary) Hypothyroidism |
Treatment is to replace the deficiency with levothyroxine. The dose is typically calculated by weight, and NICE recommend 1.6 micrograms per kilogram per day for individuals under 65 and no history of cardiovascular disease – patients with cardiovascular disease are typically started on lower doses of 25 micrograms which is then titrated up.
TSH is measured every 3 months until levels stabilise, and this is then reduced to once annually. Remember to check compliance in cases where thyroid hormone levels fail to improve.
A myxoedema coma is a potential complication of hypothyroidism and is a serious medical emergency. Various things may trigger a myxoedema coma such as hypothermia, infection, GI bleed, stroke, trauma, or drugs such as amiodarone. Ultimately, a particular stressor disrupts the body and without sufficient thyroid hormone, the body is unable to maintain sufficient homeostasis resulting in various signs and symptoms including:
Patients should be managed in an A-E approach, usually in a HDU/ITU environment, with definitive management focused on replacing thyroid hormone (usually intravenously), alongside IV steroid treatment in case there is an underlying cortisol deficiency and warming of the body to correct hypothermia. Patients may also require mechanical ventilation due to hypoventilation. ECG monitoring is important due to the risk of a prolonged QT.
Barrett, EJ. The Thyroid Gland – Medical Physiology. Chapter 49, 1006-1017.e2
https://www.ncbi.nlm.nih.gov/books/NBK459262/
http://www.medicinabuenosaires.com/PMID/29044016.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5980701/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4818825/
https://cks.nice.org.uk/topics/hypothyroidism/diagnosis/assessment/