There are two major types of pneumothorax – atraumatic and traumatic. The former can be further subdivided into:
A traumatic pneumothorax can occur due to an injury e.g. a stab wound, or iatrogenic e.g. during thoracic surgery.
PA and lateral chest x-rays are the recommended investigation for initially diagnosing a pneumothorax. Usually, an outline of the collapsed lung can be seen alongside absent lung markings. Sometimes, the deep sulcus sign may be visible. This describes a costophrenic angle which appears more inferiorly deep than usual and is a sign of a pneumothorax.
The size of the rim of air between the lung margin and chest wall is measured at the level of the lung hilum. Anything greater than 2cm is defined as a large pneumothorax, with anything less being a small pneumothorax.
Right Sided Pneumothorax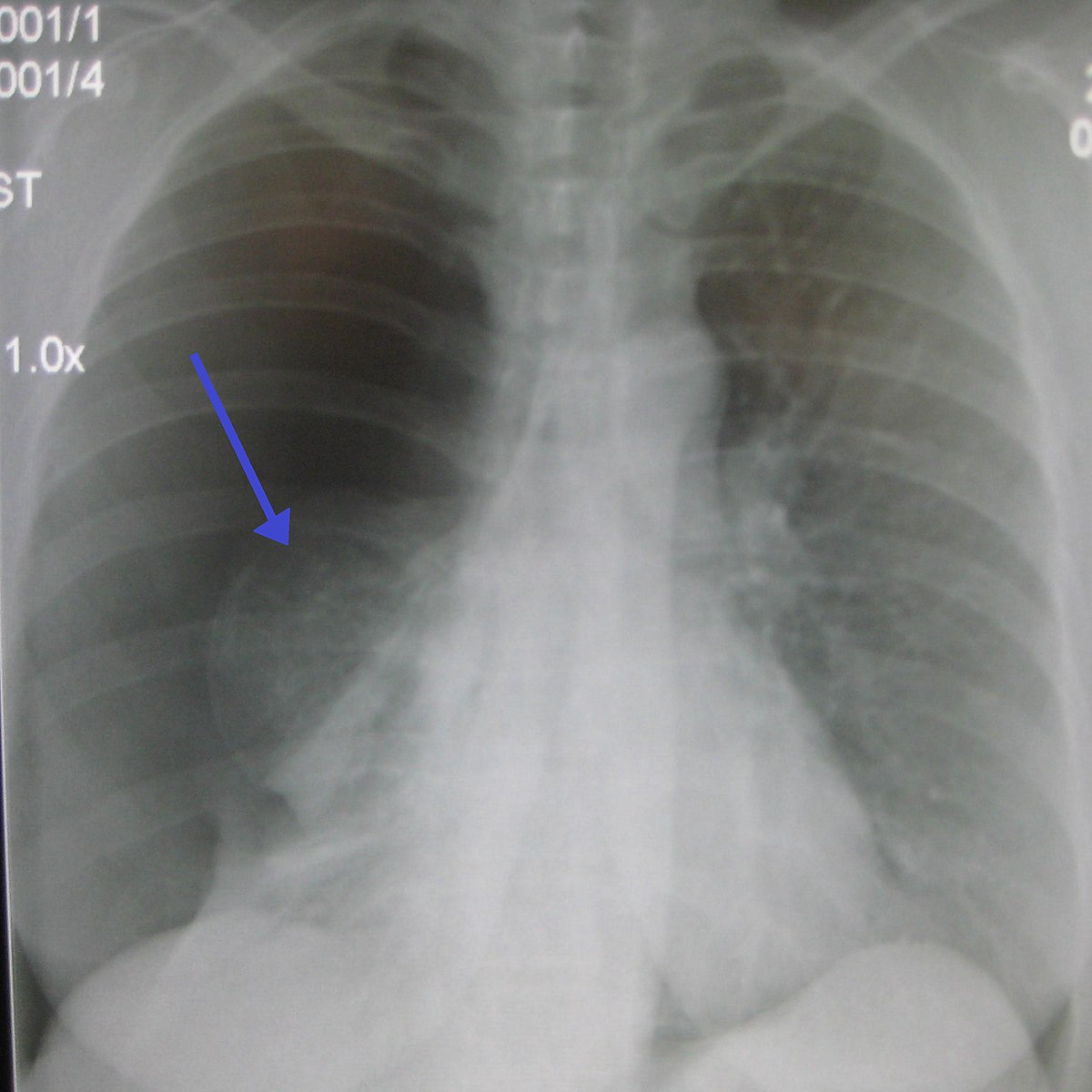
Other useful investigations include an arterial blood gas, ultrasound, or CT scan if the case is particularly complex. It is important to ensure the chest x-ray is showing a pneumothorax and not an older bulla – older imaging studies can help to make this differentiation.
Management of a pneumothorax depends on the classification. The following information is based on the British Thoracic Society guidelines, but local guidelines should also be consulted to ensure they comply with local practices.
A tension pneumothorax is an emergency situation that requires urgent and immediate management – if it is suspected e.g. from tracheal deviation, a chest x-ray should not be conducted as the patient requires urgent intervention. It is typically managed with oxygen therapy and emergency needle decompression, the latter of which involves the insertion of a cannula into the second intercostal space at the mid-clavicular line, after which a chest drain is usually inserted.
Aspiration involves inserting a 14-16G cannula into usually the 2nd intercostal space at the mid-clavicular line, or alternatively, between the 4th and 6th intercostal spaces in the mid-axillary line i.e. within the triangle of safety, or safe triangle, which describes a space between the anterior border of latissimus dorsi, the lateral border of pectoralis major, a horizontal line superior to the level of the nipple and an apex which falls at the axilla. Air is then aspirated using a syringe, and a chest x-ray can be used to confirm that the pneumothorax has been successfully drained. Needles should be inserted above the upper margin of the rib to avoid neurovascular bundle injury.
Chest drains are usually inserted between the 4th and 6th intercostal spaces in the mid-axillary line i.e. within the triangle of safety and subsequently connected to an underwater drain.
https://academic.oup.com/qjmed/article/109/9/621/1752983
https://www.ncbi.nlm.nih.gov/books/NBK441885/
https://thorax.bmj.com/content/65/Suppl_2/ii18.full
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1766017/pdf/v058p0ii53.pdf